MRI-guided stereotactic body radiotherapy (SBRT) outperforms CT guidance when it comes to reducing toxic effects of the treatment, according to a study published January 12 in JAMA Oncology.
The findings are good news for prostate cancer patients undergoing SBRT, wrote a team led by Dr. Amar Kishan of the University of California, Los Angeles.
"[Our] results demonstrated that the aggressive margin reduction afforded by MRI-guidance allowed a substantial margin reduction in acute physician-scored toxic effects as well as multiple patient-reported outcome metrics," the investigators noted.
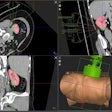
SBRT has been shown to be an effective treatment for prostate cancer, and is conducted via linear accelerator and guided by CT imaging. However, the treatment does expose men to toxic effects such as urinary, bowel, and sexual dysfunction. In theory, MRI guidance for stereotactic body radiotherapy has advantages over CT -- not the least of which being its lack of radiation and its ability to image soft-tissue and to track prostate motion directly rather than by markers that must be placed, the team explained. But MRI's benefits for this application haven't been thoroughly explored.
"Given the increased resources needed for MRI-guided radiotherapy, it is imperative to establish that it offers a tangible benefit for patients," the authors wrote.
Kishan's group sought to compare MRI-guided to CT-guided SBRT for reducing treatment margins and thus toxic effects. This research is part of phase III in an ongoing trial called MRI-Guided Stereotactic Body Radiotherapy for Prostate Cancer (MIRAGE), which enrolled 154 men undergoing SBRT for clinically significant prostate cancer between May 2020 and October 2021; all study participants had three months or more of follow-up.
The men were randomized one-to-one for SBRT with CT guidance or MRI guidance. The CT arm used planning margins of 4 mm and the MRI arm of 2 mm to deliver 40 Gy in five therapy episodes. The primary endpoint was incidence of acute (that is, within 90 days of treatment) grade 2 or greater genitourinary toxic effects (measured by a rubric called the Common Terminology Criteria for Adverse Events, version 4.03, and including cystitis, hematuria, urinary problems, and dysuria; gastrointestinal adverse events included colitis, constipation, nausea, hemorrhage, and rectal pain).
The researchers found that MRI-guided SBRT prompted fewer grade 2 or higher adverse events compared with CT-guided treatment.
| Comparison of CT- and MRI-guided SBRT for incidence of toxic adverse events | ||
| Measure | CT | MRI |
| Incidence of any grade 2 or greater genitourinary adverse event | 43.4% | 24.4% |
| Incidence of any grade 2 or greater gastrointestinal adverse event | 10.5% | 0% |
MRI-guided SBRT shows promise, but more research is needed to confirm its benefits, according to Kishan and colleagues.
"Whether the robust differences [between CT and MRI] in short-term toxic effects will persist in the longer term will require additional follow-up," they concluded.