MRI has shown that racial disparities in cerebrovascular disease begin to manifest in midlife, especially in Black individuals, according to a study published November 14 in JAMA Neurology.
The findings further underscore that people of color face serious challenges that affect the quality of their health as they age, noted a team led by Indira Turney, PhD, of Columbia University in New York City.
"Exposure to conditions that increase stress and risk for poor health, such as material hardship, interpersonal discrimination, institutional racism, residential segregation and pollution, and personal danger, are more common among Black and Latinx people than among white people," the team wrote. "[Repeated] exposure to stress, suboptimal environments, and social disadvantage contributes to accelerated wear and tear on the body, leading to a faster rate of biological aging in Black and Latinx people."
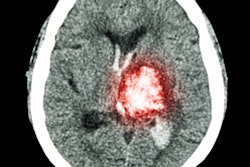
Lesser cortical thickness is a marker of degeneration of brain health and risk of Alzheimer's, while higher white-matter hyperintensity volume is associated with small-vessel cerebrovascular disease and thus risk of stroke, cognitive decline, Alzheimer's disease, and rate of Alzheimer's progression. Previous studies have found poorer brain health in Black, Indigenous, and people of color (BIPOC) individuals in later life compared with their white counterparts, but more research is needed to determine the quality of brain health in this population at midlife, Turney's team wrote.
The group explored racial and ethnic differences in cortical thickness and white-matter hyperintensity volume in midlife and late life, using MRI data from two community-based studies: the Washington Heights-Inwood Columbia Aging Project (WHICAP) and the Offspring Study of Racial and Ethnic Disparities in Alzheimer Disease (Offspring).
The final cohort included 1,467 participants, of which 33.9% were from the Offspring study and 66.1% were from the WHICAP study. Participants were assessed for comorbidities such as diabetes, high blood pressure, heart disease, and stroke; all underwent brain MRI exams.
The WHICAP group's demographic consisted of 34.8% Black, 40.1% Latinx, and 25.1% white participants, while the Offspring group's demographic consisted of 23.5% Black, 70% Latinx, and 6.4% white.
The team found the following:
- Racial and ethnic differences in cerebrovascular disease appeared in both midlife and late life, while disparities in cortical thickness appeared only in late life.
- Black-white disparities for both cerebrovascular disease and cortical thickness were greater than Latinx-white disparities, and Black-Latinx differences for these measures were slight.
- Brain aging was greater at midlife in Black individuals compared to their Latinx and white counterparts.
Differences in disease manifestation and progression due to racial and ethnic factors must be mitigated, according to the investigators.
"Future efforts will further disentangle the mechanisms underlying potential racial and ethnic disparities in brain aging, which in turn, may improve early detection, diagnosis, and treatment of [conditions such as] Alzheimer's disease," they concluded.