Women with inflammatory breast cancer have a higher risk of cancer spreading to the brain, but surveillance MRI could potentially aid in early detection of such spreading, a study published October 10 in Cancer found.
A team led by Dr. Laura Warren from the Dana-Farber Cancer Institute in Boston found that women with triple-negative inflammatory breast cancer and visceral metastasis, as well as women who are younger at diagnosis of metastatic disease, are at significant risk of having the cancer metastasize to the central nervous system. They also highlighted MRI's role in developing a treatment strategy in these cases.
"It [study] emphasizes the need to obtain brain imaging in patients with inflammatory breast cancer presenting with neurologic symptoms given the high incidence of brain metastases in this population," Warren told AuntMinnie.com.
While evidence exists showing the ties between breast cancer and central nervous system metastasis, these studies are limited by the rarity of such cases.
Managing these kinds of brain metastases is guided by numerous factors. These factors include the number and size of intracranial metastases, patient performance status and prognosis, and whether the intracranial disease is symptomatic. Radiotherapy and surgical resection are the recommended treatment options. Consensus guidelines by the National Comprehensive Cancer Network do not recommend routine MRI screening of the brain to evaluate such metastasis.
The Warren team wanted to assess risk factors and the incidence of central nervous system metastasis in women with inflammatory breast cancer as well as estimated survival after a diagnosis. They also wanted to explore trends in the use of surveillance brain MRI and describe treatment patterns in using whole-brain radiotherapy over time.
Using retrospective data, the researchers identified a total of 531 women diagnosed with inflammatory breast cancer between 1997 and 2019. Of these women, 372 had stage III cancer and 159 had de novo stage IV disease.
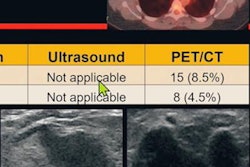
Out of the total, 124 women who had central nervous system metastasis were identified. Of these, 102 had parenchymal metastases and 35 had leptomeningeal disease, with 20 having both. The median age at diagnosis was 51 years.
| Incidence of brain metastases tied to inflammatory breast cancer by follow-up period | |||
| One year | Two years | Five years | |
| Stage III breast cancer | 5% | 9% | 18% |
| Stage IV breast cancer | 17% | 30% | 42% |
Of the total, 258 women (49%) died during observed follow-up, including 83% (103/124) of women with central nervous system metastasis. Researchers also found that the median overall survival after a diagnosis of this metastasis was 0.6 years. Women diagnosed with inflammatory breast cancer between 2000 and 2008 had a median survival after metastasis diagnosis of 0.6 years. This also applied to women diagnosed in 2009 or later.
The team also looked at risk factors for metastasis, measured by hazard ratios (HR). Triple-negative breast cancer was the biggest risk factor for developing metastases in women with stage III inflammatory breast cancer at diagnosis who underwent surgery (HR 1.98) and for women with stage IV cancer who did not present with metastases (HR 2.27).
For the latter condition, visceral metastasis had an HR of 1.96, significantly higher than that of soft tissue or serosa.
Also, 52% of the women who presented with stage III cancer were age 50 and younger, while 45% of women in this age range presented at stage IV.
For treatment trends, whole-brain radiation therapy saw a large decline from 73% from 1997 to 1999 to 46% from 2015 to 2019. Researchers also noted a "stable" number of patients being diagnosed with symptomatic metastasis over the study period, which suggests there was not an increase in the use of surveillance brain MRI over time.
The study's authors wrote that there may be more metastatic cases than suggested by their study due to the likelihood of undetected asymptomatic central nervous system metastasis. They added that early detection through surveillance brain MRI could make way for identifying limited intracranial disease burden. This would allow for focal local therapy with surgery or stereotactic radiosurgery, authors wrote.
Warren told AuntMinnie.com that a related open, phase II, single-arm study is taking place at the Dana-Farber Cancer Institute. The study will explore the effectiveness of surveillance brain MRI in women with stage III inflammatory breast cancer.
"This study will provide prospective data on the incidence of brain metastases in patients with stage III inflammatory breast cancer, which is critical, as our study likely underreported the incidence, as patients were most often identified as having brain metastases only once symptomatic," Warren said. "It will also provide valuable quality of life data."
Brain MRI could overcome barriers such as cost-effectiveness and the potential risk of overdiagnosis, according to an accompanying editorial written by Ajay Dhakal of the University of Rochester Medical Center and Dr. Carey Anders of the Duke University Health System.
The two wrote that routine brain MRI screening could identify patients with smaller, fewer, asymptomatic brain metastases who may be candidates for more focused local therapy.
"Such an approach could lead to earlier diagnosis, avoidance of whole breast radiation therapy, and potentially circumvent the emergence of possibly permanent neurologic deficits," they added.