A machine-learning algorithm's analysis of brain MRI exams has revealed the presence of neurobiological links between dementia and psychosis, according to research published online August 3 in JAMA Psychiatry.
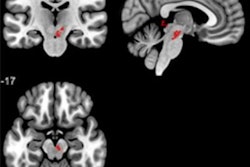
After training a machine-learning model to distinguish between healthy controls and patients with severe psychosis disorders or dementia, a multinational research group led by Dr. Nikolaos Koutsouleris of Ludwig Maximilian University in Munich, Germany, identified specific overlaps between the macroscopic brain "signatures" on MRI for schizophrenia and behavioral-variant frontotemporal dementia (bvFTD).
"These overlaps mediated aspects of the clinical-behavioral heterogeneity of both conditions, i.e., a negative avolitional syndrome in the former, and a potentially neuroinflammation-associated phenotype involving neurocognitive dysfunction in the latter," the authors wrote. "We found that the presence of bvFTD and schizophrenia patterns in patients with psychosis risk syndromes predicted impaired functional recovery."
Although severe psychotic disorders and dementia have overlapping behavioral and cognitive symptoms, it's unknown if they actually alter the brain in the same ways. In addition, researchers have not yet explored the relevance of any shared brain changes for patients in at-risk disease stages, according to the authors.
In an attempt to determine if psychosis and dementia share brain-behavioral alterations, the researchers gathered patient data from 1,870 individuals collected from January 1996 to July 2019 and analyzed between April 2020 and April 2022. Of the patients included in the study, 157 had schizophrenia, 108 had bvFTD, 102 had major depression, 96 had mild cognitive impairment or early-stage Alzheimer's disease, and 44 had established Alzheimer's disease. There were also 1,042 healthy controls.
The researchers then used machine-learning algorithms to distinguish between these patient cohorts by analyzing gray-matter volume maps on T1-weighted structural MRI exams. After deriving and comparing diagnostic patterns for these disorders, they then utilized another algorithm to assess the prognostic relevance and progression of these diagnostic patterns in 160 patients with clinical high risk for psychosis and 161 patients with recent-onset depression, comparing baseline MRI exams to an MRI exam conducted one year later.
The researchers found that the diagnostic pattern for bvFTD -- reductions in prefrontal, insular, and limbic volume -- was expressed in 65 (41.2%) of the patients with schizophrenia. Meanwhile, the schizophrenia diagnostic pattern was expressed in 92 (85.5%) of the patients with bvFTD.
"Our results support the reciprocity of brain signatures of early functional nonrecovery and neuropsychiatric illnesses," the authors wrote. "This reciprocity may point to a common final pathway of prefrontal and salience system disruption on which diverse and potentially unrelated disease mechanisms converge."
In patients with bvFTD or schizophrenia, the diagnostic pattern's progression from a baseline MRI exam to an MRI exam conducted one year later was prognostic for distinguishing between those patients who had lasting recovery compared with those who did not demonstrate recovery.
"Finally, our study revealed that young patients with poor functional outcomes overexpressed these brain patterns over time, in line with Kraepelin's concept of dementia praecox as a progressive frontotemporal disorder," the authors wrote. "Further studies into molecular disease pathways are needed to clarify how different pathophysiological processes project on overlapping neural alterations in bvFTD and schizophrenia-spectrum disorders."