Over half of women with axillary lymphadenopathy after receiving the COVID-19 vaccine continued to show the condition on follow-up ultrasound scans at 12 weeks, according to research published April 26 in Radiology.
A team led by Dr. Su Min Ha from the Seoul National University Hospital in South Korea also used ultrasound to find that vaccine-associated lymphadenopathy developed within the first two weeks of vaccination and "frequently" persisted over six weeks.
"We believe our research can provide an important clue for the radiologists and clinicians to decide their management including no recall, sufficient time for follow-up examination, or directly proceeding to biopsy," corresponding author Dr. Jung Min Chang, PhD, from the university hospital, told AuntMinnie.com.
Vaccine-related reactive lymphadenopathy is a known adverse reaction to vaccination. Research suggests that adenopathy is more commonly observed after receiving COVID-19 mRNA vaccines. And with the vaccines becoming more widely available, researchers anticipate that more patients will present with subclinical lymphadenopathy on imaging.
While ultrasound shows lymphadenopathy characteristics, there is a lack of information on the time-related changes of these imaging characteristics, how long enlarged nodes remain asymmetrically detectable, and the time to resolution on ultrasound following vaccination.
The researchers added that there is a lack of consensus on recommendations to manage lymphadenopathy observed on imaging, which could cause confusion among clinicians and radiologists.
Ha et al wanted to evaluate vaccine-associated lymphadenopathy prospectively and longitudinally on axillary ultrasound at various time intervals, in both mRNA and vector vaccine recipients.
They believed that serial follow-up ultrasound exams after vaccination could provide more information on the time-related imaging changes and how long lymphadenopathy took to resolve. They pointed out that ultrasound can be repeatedly performed without concerns of radiation or contrast agents.
The team looked at data from 88 healthy women with COVID-19 vaccine-associated lymphadenopathy undergoing serial ultrasound. A total of 49 women underwent follow-up ultrasound at a median of 12 weeks, with a range of eight to 14 weeks.
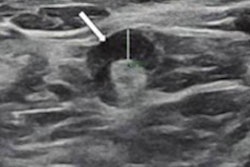
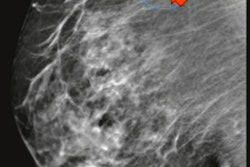
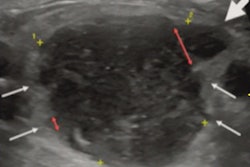
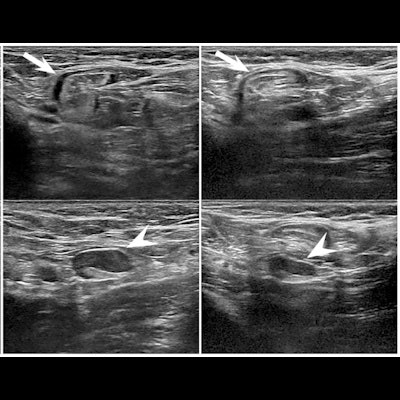
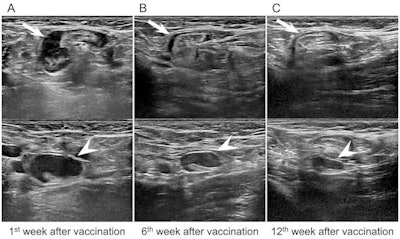 Ultrasound images of a 43-year-old asymptomatic woman without breast cancer show unilateral left axillary adenopathy after mRNA COVID-19 vaccination. (A) Images of the left axilla show enlarged lymph nodes with the cortex measuring up to 7.7 mm within the first week of BNT162b2 vaccination. (B.) Follow-up ultrasound images within six weeks (B) and (C) 12 weeks show decreased axillary lymphadenopathy of variable degrees, with the cortex measuring up to 5.7 and 3.4 mm, respectively. Image courtesy of the RSNA.
Ultrasound images of a 43-year-old asymptomatic woman without breast cancer show unilateral left axillary adenopathy after mRNA COVID-19 vaccination. (A) Images of the left axilla show enlarged lymph nodes with the cortex measuring up to 7.7 mm within the first week of BNT162b2 vaccination. (B.) Follow-up ultrasound images within six weeks (B) and (C) 12 weeks show decreased axillary lymphadenopathy of variable degrees, with the cortex measuring up to 5.7 and 3.4 mm, respectively. Image courtesy of the RSNA.After these women were vaccinated, persistent lymphadenopathy was observed in 25 women (51%). They found that complete resolution was observed at a median of six weeks, with a range of four to seven weeks, after vaccination in 23 women.
The study authors also found that nodal cortical thickness showed higher values in patients who received the mRNA vaccine than those who received the vector vaccine (p = 0.02) and gradually decreased over time (p < 0.01). However, no significant differences were found in the interaction between vaccine type and time effect.
Ha and colleagues wrote that while follow-up imaging isn't recommended for healthy women after vaccination, it may be needed for patients with recently diagnosed breast cancer or asymptomatic patients with a history of cancer undergoing monitoring.
"Although we performed this study in healthy volunteers, our finding is important and can be applicable to patients who have newly diagnosed breast cancer or personal history of breast cancer," Chang said. "In these populations, lymphadenopathy even in the contralateral axilla should be cautiously interpreted owing to the possibility of axillary metastasis or recurrence.
The team concluded that their findings can be helpful for determining best management practices for women who have recently been diagnosed with breast cancer or who have a personal history of breast cancer.
"Different time effects on complete resolution attributed to vaccine administration provide clues for deciding the time for follow-up examination or directly proceeding to biopsy in women with higher risk of metastatic lymphadenopathy," the group wrote.
In an accompanying editorial, Dr. Linda Moy and Dr. Eric Kim from New York University wrote that follow-up imaging after 12 weeks "seems reasonable" to reduce the number of follow-up examinations.
"The high incidence of adenopathy and the fact that no breast cancers were found suggest that adenopathy is a widespread and benign side effect of COVID-19 vaccinations," they added.