MRI and PSMA-PET are equally effective diagnostic tools for detecting clinically significant tumors in patients with prostate cancer, according to a study published February 16 in the Journal of Medical Imaging and Radiation Oncology.
Australian investigators compared multiparametric MRI (mpMRI) and PSMA-PET/CT with the radiotracer F-18 DCFPyL (Pylarify, Lantheus Medical Imaging) in patients with biopsy-proven prostate cancer, yet who had not undergone radiotherapy treatment. They found mpMRI and F-18 DCFPyl PSMA-PET/CT were both effective, with no statistical difference between the two approaches.
"We believe both modalities could potentially complement each other in the primary diagnosis of prostate cancer," wrote corresponding author Nishanthinie Parathithasan of the University of Melbourne in Victoria, and colleagues.
Prostate cancer is the most commonly diagnosed cancer in men. Assessing patients with biopsies can miss clinically significant prostate cancers in up to 20% of patients and diagnose clinically insignificant tumors, which can lead to overtreatment, according to the authors.
mpMRI has an established role in prostate cancer and has been shown to increase the rates of diagnosing clinically significant tumors. PSMA-PET/CT, an approach that visualizes prostate-specific membrane antigen (PSMA) on cancer cells, also has an established role in prostate cancer initial staging, yet its role in diagnosing and characterizing suspected prostate cancer is not yet clear, the authors added.
F-18 DCFPyL is a PET imaging radiotracer approved by the U.S Food and Drug Administration in May 2021 under the trade name Pylarify for the initial staging of high-risk cancer patients for therapy or in patients whose cancer appears to have returned after radiotherapy or radical prostatectomy.
In this retrospective study, the Australian group analyzed the accuracy of F-18 DCFPyL PET/CT in detecting clinically significant prostate cancer as a primary diagnostic tool and directly compared it with mpMRI in treatment-naive patients. The team then looked at whether the two approaches were better in combination than either one alone.
The group included 65 patients who had contemporaneous mpMRI and F-18 DCFPyL PET/CT imaging between January 2017 and March 2020 at hospitals in Melbourne and Canterbury, New Zealand. The patients had not undergone androgen deprivation therapy before imaging, or embolization, or radiotherapy. At the time of referral, 22 patients had biopsy-proven cancer and 43 had clinical suspicion of cancer.
The researchers found mpMRI and F-18 DCFPyL PET/CT detected the same index tumor (lesions with the highest cancer suspicion) in 90.8% of cases. PET detected an additional 6.2% of index lesions that were undetected by MRI, while detected an additional 3.1% lesions that went undetected by PET.
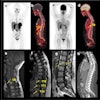
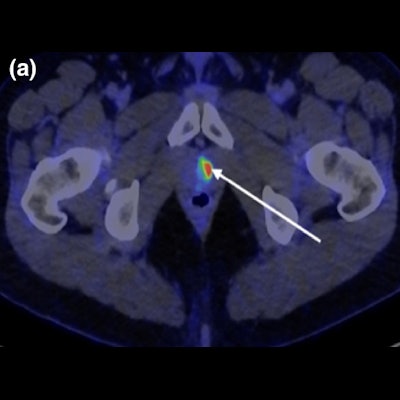
 (a) Axial fused F-18 DCFPyL PET/CT through the prostate gland apex demonstrates significant avidity in location of pathologically proven 2-mm ISUP 5 left transition zone tumor (SUVmax 10.8) (arrow). (b, c) Axial DWI B value 2000 and corresponding ADC map demonstrate no abnormal restricted diffusion within the region of PET avidity (circle). (d) Axial T2 through prostatic apex demonstrates no suspicious signal characteristics at the site of the pathologically proven ISUP 5 transition zone tumor (circle). Image courtesy of Journal of Medical Imaging and Radiation Oncology.
(a) Axial fused F-18 DCFPyL PET/CT through the prostate gland apex demonstrates significant avidity in location of pathologically proven 2-mm ISUP 5 left transition zone tumor (SUVmax 10.8) (arrow). (b, c) Axial DWI B value 2000 and corresponding ADC map demonstrate no abnormal restricted diffusion within the region of PET avidity (circle). (d) Axial T2 through prostatic apex demonstrates no suspicious signal characteristics at the site of the pathologically proven ISUP 5 transition zone tumor (circle). Image courtesy of Journal of Medical Imaging and Radiation Oncology.The sensitivity of PSMA-PET in detecting csPCa was 96.7% and that of MRI was 93.4%, with no statistically significant difference between the two (p = 0.232). In addition, no additional clinically significant prostate cancer was identified on pathology that was not seen on imaging, according to the findings.
"Both mpMRI and 18F-DCFPyL-PSMA-PET/CT have high sensitivity for detecting [clinically significant prostate cancer] with high agreement between modalities," the authors wrote.
Few studies have been published comparing PSMA-PET/CT and mpMRI for primary diagnosis, and larger prospective studies are required to validate these findings in a cohort of patients clinically suspected of having prostate carcinoma, the authors noted.
"This is currently being undertaken at our institutions," they wrote. "Further studies will be required to identify the group of patients that should undergo either both examinations or be primarily investigated with F-18 DCFPyL PET/CT," the group concluded.