Women should not delay their screening mammograms due to concerns about lymphadenopathy seen after receiving the COVID-19 vaccine, according to research published February 8 in Radiology.
A team led by Dr. Stacey Wolfson from New York University found that persistent axillary lymphadenopathy was seen up to 43 weeks after vaccination. The group suggested that radiologists interpret such lymph node swelling with a patient's risk factors in mind.
"In patients who are at lower risk [for breast cancer], it's important to realize that this is a common finding and benign reactive lymphadenopathy is something we did see very frequently with varying times of resolution," Wolfson told AuntMinnie.com.
It's become known among radiologists that lymph nodes become swollen in women presenting for breast cancer screening as a side effect of the COVID-19 vaccine, regardless of vaccine brand. However, radiologists are challenged by this since lymphadenopathy occurring on one side of the body may also point to cancer.
Lymphadenopathy caused by the vaccine usually goes away on its own and doesn't result in chronic health problems. Some previous studies suggest delaying breast screening until after swelling goes down to help women avoid false positives and unnecessary follow-ups. However, this could take several weeks in some patients.
Wolfson et al wanted to find out axillary lymphadenopathy outcomes after COVID-19 vaccination on breast images, using data from 1,217 women. They collected data from women who received the vaccine and had breast imaging between December 2020 and April 2021 at 17 sites across NYU Langone Health. They also included follow-up exams that were recorded through December 2021.
Out of the total number, 537 (44%) women had lymphadenopathy identified on at least one imaging exam. Out of these, 43 underwent a biopsy, with nine having malignant results.
Meanwhile, 823 women (68%) had screening exams and 334 patients had mammography and sonography performed the same day. Researchers found that out of these, mammography alone identified 29 cases (9%) of lymphadenopathy. Ultrasound alone identified 203 cases (61%) and both exams identified 102 cases (30%).
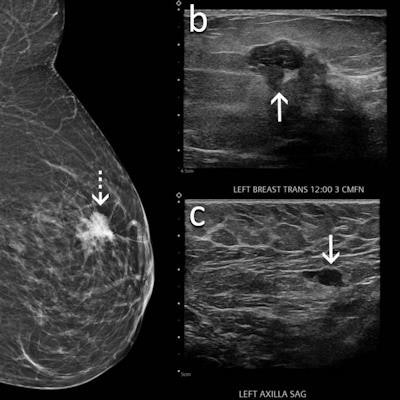
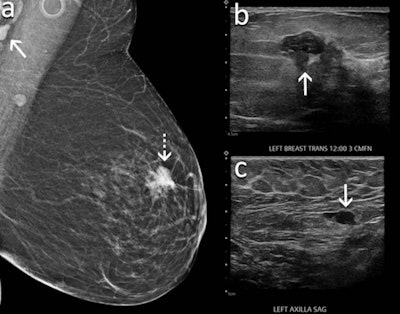 A 60-year-old woman underwent screening mammography nine weeks after receiving her second dose of the Moderna COVID-19 vaccine. (A) Mediolateral oblique view of the left breast shows an irregular mass in the superior left breast (dash arrow) and a dense lymph node in the left axilla that is incompletely visualized (arrow). Sonography meanwhile showed (B) an irregular hypoechoic mass in the breast (arrow) that corresponded to the mammographic finding and (C) a lymph node with eccentric cortical thickening measuring 6 mm (arrow) in the axilla. Biopsy of the mass showed invasive ductal carcinoma and biopsy of the lymph node showed metastatic carcinoma. Image courtesy of RSNA.
A 60-year-old woman underwent screening mammography nine weeks after receiving her second dose of the Moderna COVID-19 vaccine. (A) Mediolateral oblique view of the left breast shows an irregular mass in the superior left breast (dash arrow) and a dense lymph node in the left axilla that is incompletely visualized (arrow). Sonography meanwhile showed (B) an irregular hypoechoic mass in the breast (arrow) that corresponded to the mammographic finding and (C) a lymph node with eccentric cortical thickening measuring 6 mm (arrow) in the axilla. Biopsy of the mass showed invasive ductal carcinoma and biopsy of the lymph node showed metastatic carcinoma. Image courtesy of RSNA.Lymphadenopathy was seen as early as one day following the first vaccine dose and as late as 71 days following the second dose. The average lymph node size was 1.8 cm.
Four patients were diagnosed with metastatic breast cancer, all of whom had suspicious concurrent mammographic findings in the breast on the same side of the body where the vaccine was given. Four other women were diagnosed with lymphoma, and one patient with a known history of lung cancer was diagnosed with lung cancer metastatic to an axillary lymph node.
The researchers also found that 387 women with lymphadenopathy had a total of 407 follow-up imaging exams, on average 15.7 weeks after their first exam visits. Out of these, 323 exams were deemed to be benign while 84 were "probably benign" with recommendation for further follow-up. However, no follow-up patients had a malignant diagnosis.
The team called this the largest study to evaluate axillary lymphadenopathy, with a long-term follow-up of six months following the COVID-19 vaccination.
"We have robust, long-term follow-up data that wasn't available as the vaccines were newer. It's important because it gives us ... reflective information about what we expect to happen," Wolfson said.
While delays in cancer screening could result in consequences for women, the researchers said delays in screening caused by the pandemic will be more impactful than delays caused by lymphadenopathy.
"So many women were not able to have screening mammograms or were not willing to take risks in having screening mammograms during the pandemic itself," Dr. Beatriu Reig from NYU Langone Health told AuntMinnie.com. "I don't think the four-to-six-week screening delay that was recommended at the beginning of the vaccination has had as much of an impact on population health as the pandemic has."
While future research has not been determined, Wolfson and Reig said it would be "interesting" to further find out resolution times, anatomy, and physiology for lymphadenopathy, as well as longer-term follow-up results and rarer imaging findings.