PET/MRI is superior to MRI alone for detecting disease in patients with recurrent prostate cancer, according to a study by researchers from Weill Cornell Medicine in New York City, published October 11 in Translational Oncology.
The researchers compared the overall diagnostic performance of PET/MRI with a gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA)-11 radiotracer versus conventional, multiparametric MRI (mpMRI) for detecting lesions in patients whose cancer returned after treatment. PSMA PET/MRI is a significantly better imaging modality, they found.
"PSMA PET/MRI is a better imaging modality in the detection of disease in the setting of [biochemical recurrence] when compared with MRI alone. Combined utility with PSMA PET/MRI is a powerful tool which can aid in not only the detection of disease, but also guide in treatment planning for prostate cancer patients," wrote first author Dr. Juana Martinez and colleagues.
Prostate cancer is the most common cancer in men. About 250,000 men are expected to be diagnosed in 2021 alone and 30% of these patients are expected to experience a return of cancer after treatment, commonly referred to as biochemical recurrence.
A major marker for recurring cancer is prostate-specific antigen (PSA) produced by prostate cancer cells circulating in the patient's blood. Clinically, prostate cancer is considered recurrent if PSA levels are equal to or greater than 0.2 ng/mL after surgery or radiation therapy.
Ga-68 PSMA is a PET tracer approved by the U.S. Food and Drug Administration in December 2020 for prostate cancer patients with suspected metastases, as well as in patients with suspected recurrence based on elevated PSA levels.
Previous studies have shown that both PSMA-PET/MRI and multiparametric MRI have high detection rates in detecting pathologic lesions in patients with low PSA levels. However, studies have yet to illustrate the value of PSMA PET/MRI when compared with multiparametric magnetic resonance imaging (mpMRI), the authors stated.
In this study, Martinez and colleagues enrolled 108 patients with recurrent prostate cancer who were referred to the study by their primary oncologist, radiation oncologist, or urologist, between April 2018 to May 2021 at New York Presbyterian Hospital. The patients had undergone either radical prostatectomy, radiation therapy, or both.
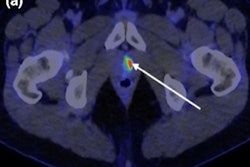
Participants received a single intravenous dose of Ga-68 PSMA-11 followed by a PET/MRI scan (Biograph mMR, Siemens Healthineers) or multiparametric MRI scans 90 minutes after injection. The PSMA PET/MRIs were reviewed by two nuclear radiologists, while the MRI head, neck, chest, abdomen, and pelvis scans were read by two diagnostic radiologists.
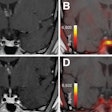
The researchers found that the number of positive reads with PSMA PET/MRI was higher than MRI for biochemically recurrent patients by a statistically significant margin. The pattern was demonstrated when reviewing the number of abnormal N1 lymph nodes, N2 lymph nodes, osseous, prostate/prostatic bed, and other lesions. MRI detected more abnormal lesions in the prostate.
| PSMA PET/MRI vs. mpMRI for detecting lesions by location | ||
| MRI | PSMA PET/MRI | |
| N1 | 9.65% | 29.8% |
| N2 | 6.14% | 17.5% |
| Osseus | 12.3% | 21.1% |
| Prostate | 6.14% | 2.63% |
| Prostatic bed | 6.14% | 7.01% |
| Other | 0.01% | 2.63% |
In addition, PSMA PET/MRI was more likely to have a positive read than MRI at all PSA levels. In patients with serum PSA levels < 0.2 ng/mL, PSMA PET/MRI was positive in detecting a suspicious lesion within the chest, abdomen, and pelvis in 32% of patients while MRI was positive in only 9% of patients.
"Our findings demonstrate that PSMA PET/MRI is a better imaging modality in the detection of disease in the setting of [biochemical recurrence] when compared to MRI alone," the team wrote.
The authors noted a limitation of the study is that multiple patients sought care at other institutions either prior to the PET/MRI scan or after and as a result, the information was not complete for several patients enrolled in this trial. Only a small number of the subjects had a follow-up or underwent confirmatory biopsy, which introduces the possibility of selection bias for this subset, they wrote.
"Future studies should evaluate the role of PSMA PET/MRI with MRI in the detection of biochemical recurrence after radiation therapy in a larger cohort," the authors concluded.