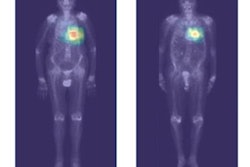
PET imaging is more effective than bone scintigraphy for detecting metastatic disease in children with soft-tissue cancer, according to a study published online August 9 in the European Journal of Cancer.
A group of researchers from five European countries investigated the impact of F-18 FDG-PET/CT compared with standard radiology workup in pediatric and young adult patients with rhabdomyosarcoma, an aggressive cancer that forms in skeletal muscle tissue. The team found PET/CT was more sensitive identifying cancer lesions than bone scintigraphy.
However, standard radiology workup also includes the use of MRI and chest CT, which remain essential tools when evaluating these patients, the study authors noted.
"Our study demonstrates that F-18 FDG-PET/CT has a higher capacity to detect lymph node and bone involvement and can replace the use of bone scintigraphy," they wrote.
Rhabdomyosarcoma (RMS) is a highly aggressive tumor and is the most typical form of soft-tissue sarcoma in children and young adults. It accounts for up to 5% of all childhood malignancies, with an incidence of 5.3 per million children under the age of 15 per year.
The European Pediatric Soft Tissue Sarcoma Study Group was formed in 2005 with the goal of standardizing the treatment of soft-tissue sarcoma in pediatric patients. The group conducted a prospective, multi-institutional clinical trial in 74 centers in 11 countries from October 2008 to December 2016 in patients with localized RMS.
When the study was launched, F-18 FDG-PET/CT was considered optional, but use of the modality has been growing based on positive reports in adult sarcomas patients. In this study, the group performed a retrospective analysis of the impact of F-18 FDG-PET/CT in patients who received imaging.
Among 263 metastatic patients enrolled from October 2008 to December 2016, 121 had PET-CT performed at diagnosis, and for 118 of 121 patients, both PET-CT and radiological reports were available for review.
PET-CT showed higher sensitivity than standard radiology workup in the ability to detect locoregional (96.2% vs. 78.5%) and distant lymph node involvement (94.8% vs. 79.3%), but sensitivity was lower for intrathoracic sites (lung 79.6% vs. 100%).
Standard radiology workup found 223 metastatic sites, while F-18 FDG-PET/CT identified 229, with a mean number per patient of 1.72 for standard workup and 1.94 for F-18 FDG-PET/CT.
The researchers identified 46 patients who had both 18F-FDG-PET/CT and bone scintigraphy at diagnosis. Comparing the role of in the detection of bone metastases, F-18 FDG-PET/CT identified lesions with a higher sensitivity but lower specificity.
| FDG-PET/CT vs. bone scintigraphy for bone metastasis in RMS patients | ||
| Bone scintigraphy | PET/CT | |
| Sensitivity | 82.6% | 95.6% |
| Specificity | 100% | 78.2% |
In addition, in four patients (3.4%), PET-CT changed the staging from localized to metastatic disease.
The data supports replacing bone scintigraphy with F-18 FDG-PET/CT in RMS, given it will increase the number of metastatic patients identified, the authors stated.
However, they also found MRI of the primary tumor remains essential for evaluating primary tumor size and extent, and chest CT exploration is essential to search for intrathoracic lesions in the group, the researchers wrote.
Ultimately, the strength of the study is that it provides the largest series to date on the use of F-18 FDG-PET/CT in the staging of metastatic RMS in a pediatric population, according to the authors.
"F-18 FDG-PET/CT has been included in the standard staging investigations, and a randomized trial will try to evaluate the prognostic value of F-18 FDG-PET/CT response and its potential use as imaging biomarker," the group concluded.