Quantitative 3D analysis of weight-bearing CT is a promising technique for assessing the structural changes associated with knee osteoarthritis (OA), according to research published online April 13 in Radiology.
Using internally developed 3D image visualization software, a multinstitutional team of researchers led by Dr. Tom Turmezei, PhD, of Norfolk and Norwich University Hospitals NHS Foundation Trust in the U.K. found that 3D maps of the knee joint space width distribution correlated highly with structural joint disease. Taking less than 10 minutes to perform, the method was feasible and reproducible, detecting joint space width differences as low as ± 0.1 mm.
"It is reliably learned by novice users, can be personalized for disease phenotypes, and can be used to achieve a smallest detectable difference that is at least 50% smaller than that reported to be achieved at the highest performance level in radiography," the authors wrote.
Although imaging of structural disease in osteoarthritis has traditionally been the domain of MRI and radiography, conebeam CT can now be used to acquire knee images in a standing position. By offering 3D assessment of joint space width, CT could yield higher sensitivity than radiography for detecting disease-relevant structural changes, according to the researchers.
In their study, the researchers used the free StradView 3D software to segment, reconstruct, and create 3D joint space maps on weight-bearing CT images acquired on a LineUp conebeam CT scanner (CurveBeam). They tested the reproducibility of the technique in 20 individuals and its repeatability in nine subjects from the Multicenter Osteoarthritis Study.
After performing limits of agreement analysis, they found that the method could detect width differences of less than ± 0.1 mm in the central medial and lateral joint spaces, a smaller detectable difference than the ± 0.2 mm previously reported in the literature as the minimum measurement of joint space width on radiography, according to the authors.
The researchers also found that the average root mean square coefficient variation was less than 5% across all study groups.
In addition, statistical parametric mapping performed on 33 individuals revealed that the central-to-posterior medial joint space was significantly narrower by 0.5 mm (threshold p < 0.05) for each incremental increase in the patient's Kellgren-Lawrence grade.
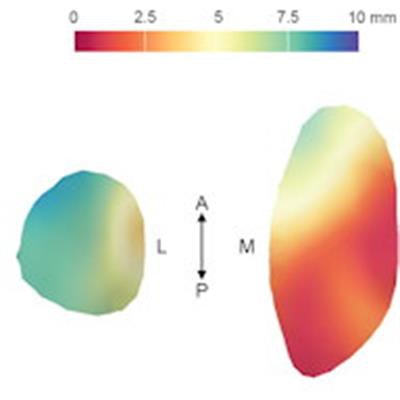
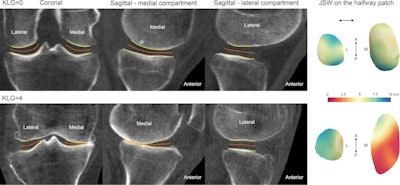 Articular bone surfaces at the femur and tibia from joint space mapping output (yellow) with the halfway surface (orange), alongside joint space width (JSW) displayed on the halfway patches (far right). This is shown for individuals with a radiographic Kellgren-Lawrence grade (KLG) of 0 (top row) or 4 (bottom row), demonstrating robust performance in the extremes of the disease. A = anterior, L = lateral, M = medial, P = posterior. Image and caption courtesy of the RSNA.
Articular bone surfaces at the femur and tibia from joint space mapping output (yellow) with the halfway surface (orange), alongside joint space width (JSW) displayed on the halfway patches (far right). This is shown for individuals with a radiographic Kellgren-Lawrence grade (KLG) of 0 (top row) or 4 (bottom row), demonstrating robust performance in the extremes of the disease. A = anterior, L = lateral, M = medial, P = posterior. Image and caption courtesy of the RSNA.Also, one patient with a Kellgren-Lawrence grade of 2 had a 24-month change in a patient's 3D joint space width distribution that was beyond the smallest detectable difference across the lateral joint space, according to the researchers.
In an accompanying editorial, Dr. Frank Roemer of Friedrich Alexander University Erlangen-Nürnberg in Germany said that the research is an important step forward in validating the use of weight-bearing CT in evaluating structural parameters relevant to OA progression.
Open questions remain, however, including determining if the loss of 3D joint space width on weight-bearing CT has a predictive role or if it's just concurrent with worsening of physical function and joint structure as shown on radiographs or MRI scans, he said.
In addition, a positioning device is required to guarantee standardized image acquisition and reproducible data. Comparability of the method with identical knee flexion between time points is also still necessary, he said.
"Additional potential applications in the context of knee OA include the use of [weight-bearing] CT arthrography for detailed evaluation of meniscal abnormalities and the chondral surface under loading conditions," Roemer wrote. "Once some of these open questions have been addressed, [weight-bearing] CT has the potential to develop into a mature technique with an established role in the clinical assessment of knee OA."



















