Breast MRI may be the most sensitive imaging modality available for detecting breast cancer, but it has its pitfalls: namely, a unique set of perceptual and cognitive errors that result in false negatives, according to an article published online March 19 in RadioGraphics.
What can radiologists do to avoid them?
The first step is understanding why false-negative findings occur in breast MRI, wrote a group that included first author Dr. Katrina Korhonen and senior author Dr. Emily Conant, all from the Hospital of the University of Pennsylvania. The authors also discussed a few strategies to avoid these diagnostic pitfalls in the future, categorizing the main types of errors as perceptual or cognitive.
Perceptual errors are the most common type of error in diagnostic radiology, reportedly accounting for up to 80% of errors. A perceptual error occurs when an abnormality is identified only retrospectively and was not detected prospectively. The finding is simply not detected.
Several types of perceptual errors can occur in breast MRI:
- Failure to detect owing to blind spots or poor search patterns
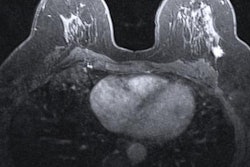
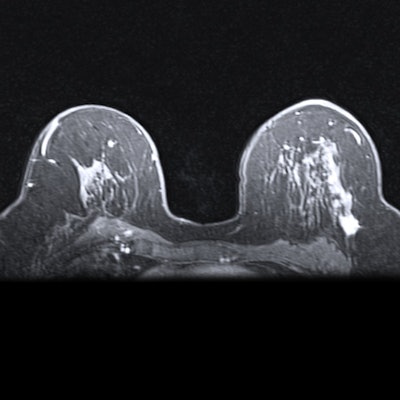
- Poor lesion conspicuity (including small lesion size, poor conspicuity secondary to a complex background parenchymal pattern, or obscuration or reduced visualization due to background parenchymal enhancement)
- Subtle or atypical appearance of cancer
- Satisfaction of search
- Reader fatigue, distractions, or interruptions
To combat poor lesion conspicuity, careful review of the maximum intensity projection (MIP) images, as well as axial or sagittal reconstructed images, is critical. Small foci not apparent in one projection may become more visible when viewed in another imaging plane.
A review of the first postcontrast sequences is also helpful for identifying small malignant lesions, as the difference in lesion-to-background enhancement is greatest at this time point, the group added.
Cognitive errors, on the other hand, occur when an abnormality is identified but misinterpreted or mischaracterized as benign. Common causes of cognitive errors include a lack of medical knowledge, radiologist bias, and incorrect or incomplete clinical information.
Types of cognitive errors include the following:
- Stable or slow-growing lesion
- Lesions with seemingly benign features (including benign shape, morphology, or T2 hyperintensity)
- Attributing a suspicious finding as secondary to postsurgical change
- Incorrect or misleading clinical information
- Lack of knowledge (including failing to recognize that not all cancer subtypes may be visualized at MRI)
- Radiologist bias
Although certain features of masses at MRI may suggest they are benign, such as a round or ovoid shape, circumscribed margins, or "persistent" enhancement patterns, these features can also be associated with malignancy, particularly in patients who are BRCA mutation carriers, for instance.
To avoid cognitive errors, readers should ensure they obtain a thorough clinical history, review all imaging sequences in all planes, and use all available comparison examinations to detect subtle changes over time.
Finally, technical errors are also important to consider. Common types include the following:
- Patient motion
- Lack of intravenous contrast material administration (including unrecognized contrast extravasation)
- Incomplete or inadequate visualization of findings on images (due to poor patient positioning or secondary to a finding being located at the edge of or partially excluded from the field-of-view)
- Artifacts (including those from metal or hematoma)
Ideally, MRI technologists can counsel patients before exams regarding the importance of remaining as still as possible and should also ensure patient comfort by helping secure the patient's arms and head in place with pillows. Some authors have reported better technique by imaging the patient in an arms-down position, rather than having the patient's arms extended above the head, noting that the position may be easier to hold, Korhonen and colleagues wrote.
Even though MRI remains the most sensitive modality for diagnosing breast cancer, some false-negative results will occur.
"A small number of false-negative cases are inevitable, as certain cancers may not demonstrate significant contrast enhancement," the group concluded. "While breast MRI represents a valuable diagnostic tool, it is important that radiologists recognize the potential limitations of the modality to avoid missed cancers."