A new, 200,000-patient review suggests that 2D images reconstructed from digital breast tomosynthesis (DBT) may be able to adequately replace digital mammograms. The Canadian team behind the paper published their findings on September 23 in the American Journal of Roentgenology (AJR).
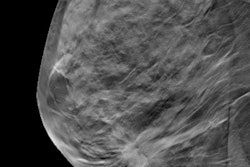
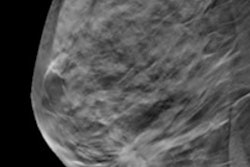
DBT has become increasingly popular for screening and diagnostic mammography, thanks to better recall and cancer detection rates than older, 2D breast imaging techniques. Nevertheless, 2D imaging is still important for evaluating breast tissue patterns and findings in multiple slices.
In the new study, lead author Peri Abdullah, PhD, and colleagues found that synthesized 2D mammograms re-created from DBT acquisitions were just as accurate as those acquired with traditional digital mammography. The findings suggest that clinicians may be able to use just one scan for both 3D and 2D breast imaging, noted Dr. Reni Butler, a radiologist at Yale School of Medicine.
"This study supports utilization of digital breast tomosynthesis as a single acquisition-examination, without a second radiation exposure to obtain a conventional 2D digital mammogram," Butler wrote in an invited commentary, which was also published on September 23 in AJR.
For their review, Abdullah and colleagues searched the scientific literature for studies of patients undergoing synthesized 2D mammograms (SM) and conventional digital mammograms (DM) with and without additional DBT imaging. Thirteen studies met their inclusion criteria for a total study population of 201,304 patients.
| Accuracy of 2D breast imaging modalities | ||||
| DM alone | Synthesized 2D alone | DM + DBT | Synthesized 2D + DBT | |
| Sensitivity | 74% | 76% | 84% | 83% |
| Specificity | 86% | 91% | 90% | 92% |
| Accuracy | 85% | 88% | 90% | 90% |
The authors found no significant differences in sensitivity and specificity between DM and SM, either alone or in combination with DBT. They also found no significant difference in their unadjusted analyses or when adjusting for important confounding factors, such as study risk of bias, reference standard, or design.
The findings have important implications for reducing patient radiation exposure. Prior research has found that radiation dose can be reduced by roughly half when clinicians opt for synthesized 2D with DBT instead of DM with DBT.
"Reconstructing a SM image does not require additional radiation exposure beyond that required for DBT," the authors wrote. "This further supports the implementation of SM in place of DM in breast imaging with the aim of reducing radiation exposure in this patient population."
Despite its promise, the adoption of combined synthesized 2D and DBT imaging has lagged in clinical practice, Butler noted in her commentary. This is partly due to clinician concerns with synthesized images regarding decreased sensitivity for fine microcalcifications and subtle masses, as well as the presence of artificial pseudocalcifications.
Butler suggested that some modifications may make clinicians more comfortable with using synthesized 2D images in day-to-day practice. For instance, clinicians may choose to still use traditional DM for baseline screenings or to obtain a magnification view of microcalcifications.
"With these adaptations, the learning curve for incorporating SM into clinical practice and achieving an acceptable level of comfort with it can be reasonably short," she concluded.