A Medicare payment model in Oregon that reimbursed certain community health clinics based on their total number of patients instead of their volume of patient encounters led to a drastic decline in the number of imaging procedures, according to the findings of a study published on July 7 in Health Affairs.
Community health clinics that participated in the program had a 42% decline in price-weighted primary care services, a drop that was almost entirely attributed to a decrease in imaging services such as radiography and ultrasound.
 Stephan Lindner, PhD. Image courtesy of OHSU.
Stephan Lindner, PhD. Image courtesy of OHSU."These types of easily quantifiable and billable services are often overused when payment structures incentive a high volume services, and they are a leading contributor of low-value care," wrote the authors, led by Stephan Lindner, PhD, an assistant professor at Oregon Health & Science University (OHSU) in Portland, OR.
In 2013, Oregon introduced an optional Medicaid payment program that switched from a fee-for-service-like model to one that paid for services based on the total number of Medicaid patients who used a clinic for primary care.
The researchers used Medicaid claims data to compare the volume of services rendered by community health centers that participated in the new payment program and clinics that stuck with the old payment model.
The price-weighted volume for all traditional primary care services declined significantly for clinics that participated in the new program. The mean price-weighted volume of all services fell by $13.1 per member per month in the first year after a clinic joined the program and $14.9 per member per month the second year.
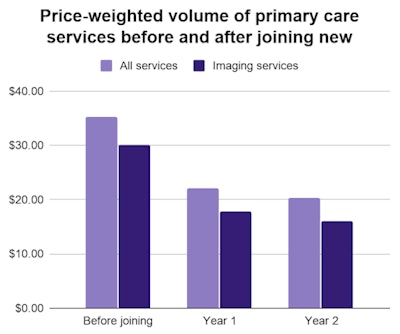
That decline in the price-weighted volume of services was fully attributed to a decrease in price-weighted imaging services, including radiography and ultrasound, according to the authors. The price-weighted volume of imaging services fell by $12.3 in the first year and $14.1 in the second year.
Importantly, the price-weighted volume of services, including imaging services, did not change for clinics not participating in the new payment program. The results were also similar when the researchers looked at imaging services provided by outside facilities in a sensitivity analysis.
"Before its implementation, reimbursement was tied to face-to-face encounters, which created an incentive for a high number of visits," the authors wrote. "The shift to a flat per member per month rate for attributed Medicaid patients eliminated this incentive and led to a decline in the services provided at [clinics.]"
The authors hypothesized that the decline in imaging was because there was less of an incentive to obtain imaging in the new payment model. It could also be because clinics had more same-day appointments available, reducing the need for imaging services.
"The point of the reform is to reduce services that aren't super valuable so that clinics can free up resources to get people the services they need," stated Lindner in a press release. "It frees up clinics toward services that can engage these patients in a different way, such as telephone consultations and basic health screenings."