Interventional radiology is in a prime position to leverage the enhanced visualization afforded by augmented reality (AR) technology to improve image-guided procedures and achieve better outcomes, according to a recent article published online in the Journal of Vascular and Interventional Radiology.
"Augmented and mixed reality are novel display technologies that are able to provide a new way to visualize images and localize targets during image-guided procedures," wrote the authors, led by Dr. Brian Park and Dr. Stephen Hunt, PhD, of Penn Medicine.
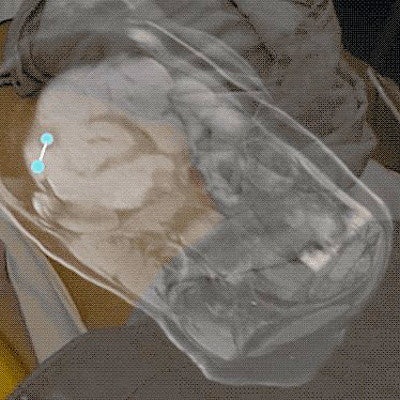
 Augmented reality visualization based on MR images of a patient's metastatic neuroendocrine tumor. Interventional radiologists used augmented reality technology to plan their surgical approach for liver microwave ablation. Video and image courtesy of Dr. Brian Park.
Augmented reality visualization based on MR images of a patient's metastatic neuroendocrine tumor. Interventional radiologists used augmented reality technology to plan their surgical approach for liver microwave ablation. Video and image courtesy of Dr. Brian Park.AR's capacity to enhance the visualization and localization of targets has shown in recent studies that it can help produce a wide range of benefits, from enhancing anatomic understanding to reducing radiation exposure and operation times, they noted.
"Although interventional radiology has been somewhat slow to adopt such technologies, these technologies may be appealing to interventional radiologists and image-guided therapists for readily accessible image viewing or advanced 3D visualization intraprocedurally," they wrote (J Vasc Interv Radiol, February 12, 2020).
New visualization technology
One of the main advantages of AR, as it pertains to interventional radiology, is that it allows users to overlay holograms onto real-world objects anywhere within the surgical suite and interact with them without losing sight of the natural environment. Clinicians have been applying this use of AR to medical training and education at a growing rate over the past several years.
For example, interventional radiologists have used AR to create immersive scenarios to simulate procedures for complex cases and test new equipment, according to the authors. AR has also allowed radiologists to offer and receive assistance from other experts in real-time -- ideal for collaborating with those in rural or developing regions.
The benefits of AR extend to other interventional radiology staff members as well, they continued. AR-assisted virtual C-arm positioning guides have helped aid radiologic technologists in establishing proper C-arm views more quickly than manual positioning, reducing their exposure to radiation. In addition, clinicians can use AR technology to project radiation dose maps onto the interventional radiology table in order to monitor all staff members' radiation exposure during procedures.
More recently, advancements in AR technology have enabled researchers to create holograms with near-perfect calibration accuracy to the original medical imaging data. This has paved the way for the intraoperative use of AR for a wide range of interventions, such as spinal joint injections and various cardiac procedures.
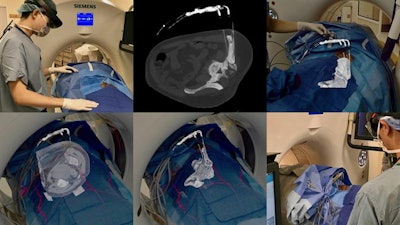 Intraoperative CT scans were projected as augmented reality holograms onto a patient undergoing cryotherapy for left iliac bone metastasis. Interventional radiologists registered the holograms to cryoablation probes on the patient and adjusted window settings in real-time to exclude soft tissue and focus on the bone.
Intraoperative CT scans were projected as augmented reality holograms onto a patient undergoing cryotherapy for left iliac bone metastasis. Interventional radiologists registered the holograms to cryoablation probes on the patient and adjusted window settings in real-time to exclude soft tissue and focus on the bone.Despite these promising qualities, AR has received less attention from interventional radiologists than it has from other specialties, the authors noted. Among 11 procedural specialties, interventional radiology has produced the fewest published studies exploring the use of AR for procedures.
"As image-guided experts and proceduralists, more experimentation and developments in interventional radiology should be undertaken to evaluate this new visualization technology as other specialties have done," the authors wrote.
Clinical applications of AR
In their review article, Park, Hunt, and colleagues examined current research efforts to integrate AR into interventional radiology. They categorized the work based on the type of interventional radiology procedure to which researchers applied AR:
- Endovascular procedures: Early work in the field has primarily centered on using AR to enhance preoperative planning for complex procedures. The 3D information provided by AR allows clinicians to visualize anatomy and pathology very quickly, compared with the standard technique of mentally reconstructing 2D images into 3D images.
- Percutaneous procedures: An increasing number of groups have developed techniques using AR to navigate percutaneous needle-based procedures. Proof-of-concept studies have demonstrated that relying on AR holograms to guide percutaneous bone interventions, liver biopsies, and similar procedures can reduce radiation dose, procedure times, and the number of images acquired.
Interventional radiologists have also used AR to look inside patients virtually from multiple viewpoints to help decide on the best approach before performing procedures. AR also enables interventional radiologists to project conebeam CT or rotational angiography data in front of them as 3D models during endovascular procedures, rather than scrolling through the 2D imaging data on a monitor.
Other studies have shown that AR can facilitate optimal probe placement for ablation procedures, lower targeting errors for needle tracking, and improve resource utilization during needle localization. In one study, researchers used AR technology to guide needle insertion into lumbar spine phantoms with high accuracy based on preoperative CT data, eliminating the need for real-time CT fluoroscopy.
Further development of AR technologies is still needed; current AR devices offer a limited field-of-view compared with natural sight and relatively short battery life, the authors noted. High-level, evidence-based clinical studies are also required to validate the benefits of AR and determine to what extent it can improve the safety and efficiency of interventional radiology procedures.
"Clinical evidence is currently lacking, but as these technologies evolve, augmented reality may become easier to implement and use in an actual volumetric fashion to enhance interventions," Park, Henry, and colleagues wrote.
Current research has shown progress and potential for "translation and adoption [of AR] into the interventional radiology suite [and] may transform the way future image-guided interventions are undertaken and provide benefits to patients, operators, and staff," they concluded.