More than a quarter of women who have breast lesions categorized as BI-RADS 3 do not receive appropriate diagnostic follow-up, according to a study published online October 26 in the Journal of the American College of Radiology.
The results suggest that determining which particular patient factors contribute to less-than-ideal tracking of BI-RADS 3 findings could help clinicians develop better interventions for women with lesions in this category, wrote a team led by Dr. Ronilda Lacson, PhD, of Brigham and Women's Hospital in Boston.
"A care coordination system that incorporates analytics and risk estimation to identify persons at high risk for suboptimal follow-up could reduce follow-up disparities," the group wrote.
About a third of diagnostic errors "involve a failure or delay in ordering, scheduling, and executing diagnostic tests, including 45% involving diagnostic imaging," and a study analyzing malpractice cases between 2009 and 2013 showed that "20% alleged a diagnosis-related error" as the reason for the suit, the researchers noted.
So because the BI-RADS 3 category is equivocal, breast lesions classified as such represent a possibly dangerous situation for both women and their doctors, according to Lacson and colleagues.
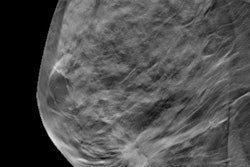
"Recommendations for category 3 breast findings on mammography typically include six-month follow-up imaging, followed by 12- and then 24-month imaging," the team wrote. "However, follow-up imaging has been suboptimal in many women. ... Because BI-RADS 3 breast lesions have up to 2% likelihood of malignancy, it is imperative that optimal follow-up of BI-RADS 3 test results be addressed to avoid this potential source of diagnostic imaging failure."
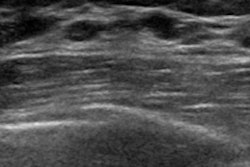
To investigate the rate of follow-up and explore patient- and provider-related factors in patients with BI-RADS 3 findings, the researchers conducted a study that included 93,685 breast imaging exams, of which 2,967 were categorized as BI-RADS 3 (4.6%) from unique patients. After researchers excluded an additional 1,456 baseline exams because they had been taken via breast MRI, had an additional breast imaging assessment within three weeks of the index exam, or had been taken elsewhere, for a cohort total of 1,511.
Of these, 74% (1,125) had optimal follow-up, 20% (305) had no follow-up, and 7% (103) had delayed follow-up (nine months or more after the initial screening exam), Lacson and colleagues found. Mean time to cancer detection was 85 days longer for women who did not receive appropriate follow-up compared with those who did; the study's cancer rate was 13 of 1,511, or 0.86%.
The authors discovered prior breast cancer and having a cancer institute as the referring provider were associated with effective follow-up of BI-RADS 3 findings, while the following factors were associated with suboptimal follow-up:
- Younger age
- Hispanic ethnicity
- Being divorced
- Lacking insurance
The suboptimal follow-up rate of 26% that Lacson and colleagues found is consistent with other research, which has shown a range of 12% to 33%, according to the authors.
"This finding is significant given the large number of women who undergo breast imaging annually," the group noted.
More research is needed, the team concluded.
"Future studies should focus on follow-up disparities so that effective interventions may be designed and implemented," the group wrote.