FDG-PET can help boost the detection of abnormalities associated with complex regional pain syndrome when clinicians turn to PET/MRI for diagnosis of the condition, according to a study presented last week at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting.
When using the hybrid modality to detect lesions in neurovascular bundles and skin thickness, Stanford University researchers found the improved sensitivity of FDG-PET discovered changes in muscle tissue that MRI could not diagnose.
"Interestingly, of those lesions, only PET was able to identify muscular changes," said lead author Daehyun Yoon, a research associate in radiology at Stanford. "Skin and some of the neurovascular bundle changes were detected by MRI as well, but in general, FDG-PET was more sensitive to inflammatory changes. Our findings suggest that FDG-PET is more sensitive to pathologic changes coming from the complex regional pain syndrome."
Extremity pain
Complex regional pain syndrome is characterized by continuing intense pain, primarily in the hands and feet. Approximately 50,000 new cases of this condition occur in the U.S. each year, and millions more people deal with the pain syndrome worldwide.
"The problem with complex regional pain syndrome is that it does not have any specific diagnosis for detecting the cause of the pain," Yoon told attendees at SNMMI 2019. "Typical complex regional pain syndrome symptoms are similar to peripheral nerve injury, but the standard methods for identifying nerve injury are invasive and can significantly exacerbate pain symptoms in complex regional pain syndrome patients."
So what are the possible noninvasive alternatives to detecting the syndrome? In previous research, FDG-PET/MRI showed promising results in the detection of painful nerve injury and associated muscle changes in both animal and human studies. Hence, Yoon and colleagues sought to use PET/MRI to detect early musculoskeletal and pathological changes due to complex regional pain syndrome. PET/MRI enabled the researchers to explore metabolic changes with PET and anatomic abnormalities with MRI.
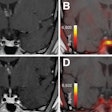
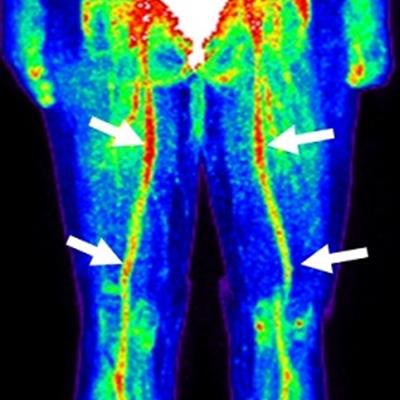
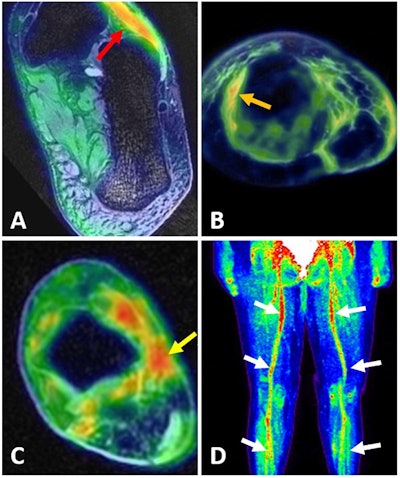 PET/MR images show high FDG uptake in dorsal foot muscle (A, red arrow); in thickened subcutaneous tissues (B, orange); on the tibial nerve surrounded by scar tissue (C, yellow arrow); and globally increased FDG uptake on femoral, popliteal, and tibial neurovascular bundles (D, white arrow). Images courtesy of Yoon et al and SNMMI.
PET/MR images show high FDG uptake in dorsal foot muscle (A, red arrow); in thickened subcutaneous tissues (B, orange); on the tibial nerve surrounded by scar tissue (C, yellow arrow); and globally increased FDG uptake on femoral, popliteal, and tibial neurovascular bundles (D, white arrow). Images courtesy of Yoon et al and SNMMI.Hybrid approach
The researchers performed FDG-PET/MRI scans on seven patients with complex regional pain syndrome in their feet, along with seven healthy controls. PET imaging was conducted one hour after injection of 10 mCi of FDG, during which time-of-flight PET also was performed. For the 3-tesla MRI portion of the scan, the researchers used a whole-body approach, which took 35 to 40 minutes to complete.
"We performed a whole-body PET/MRI because if the patient has a symptom in the foot or the hand, it does not necessarily mean that the patient's pain generator is at the hand or the foot," Yoon explained. "So we ran the whole-body PET/MRI first to open all the possibilities, and those findings were compared with healthy controls."
As PET and MRI abnormalities were identified, the researchers divided the results into three tissue types: muscle, neurovascular bundles, and skin. Maximum standardized uptake values (SUVmax) also were calculated for the detected lesions and compared with corresponding measurements from the healthy subjects.
Only the FDG-PET images detected lesions in the foot muscles of five patients (71%), with the pain symptoms located in the right dorsal foot muscles, left plantar foot muscles, and a right ankle scar. In three patients (43%), FDG uptake identified the abnormalities among neurovascular bundles in the bilateral plantar, tibial, femoral, and popliteal nerves and in the right posterior tibial nerve; MRI spotted abnormal signal on left saphenous and sural nerves. Three patients had both foot muscle and neurovascular pain issues. Finally, both FDG-PET and MRI detected thickening of the foot's skin and edema in two patients (28%).
As one might expect, mean FDG SUVmax levels were significantly higher for patients with the pain syndrome, compared with healthy subjects. (The p-value for skin was not applicable [N/A] due to small sample size.)
| Mean SUVmax results for pain patients and healthy controls | |||
| Healthy controls | Complex regional pain syndrome | p-value | |
| Muscular | 0.86 | 1.49 | 0.013* |
| Neurovascular | 0.60 | 1.40 | 0.0009* |
| Skin | 0.04 | 3.10 | N/A |
Based on the results, the Stanford researchers suggest in their SNMMI abstract that high FDG uptake on multiple neurovascular bundles might be used to "differentiate complex regional pain syndrome into a specific subtype as a surrogate marker for a potential autoimmune component of complex regional pain syndrome, which is being increasingly attributed to one of the causes of complex regional pain syndrome."