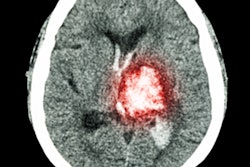
Stroke patients who underwent endovascular therapy had similar improvement after their treatment regardless of the type of perfusion imaging -- CT or MRI -- that clinicians used to confirm their eligibility for surgical procedures, according to an article published online January 28 in JAMA Neurology.
Several recent studies using perfusion imaging to examine stroke patients, including the Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke 3 (DEFUSE 3) trial, have affirmed that the time window for effective surgical treatment of stroke could be safely extended by several hours after stroke onset.
These reports have led the American Heart Association and the American Stroke Association to change their stroke therapy guidelines, which now give a level 1A recommendation for thrombectomy up to 16 hours after a stroke. Following this change, clinicians have begun to investigate the extent to which postsurgical outcomes could be affected by different variables such as patient age and the type of imaging exam the patients undergo.
"As these findings are translated into clinical practice, a fundamental question is whether ... MRI or CT perfusion is the optimal imaging modality for evaluation of late-window patients," wrote Dr. Maarten Lansberg, PhD, from Stanford University and colleagues.
In a secondary analysis of data from the DEFUSE 3 trial, Lansberg and colleagues examined the 90-day outcome of 182 stroke patients who received endovascular therapy. The median age of the patients was 70 years, 51% were women, and all of them underwent either perfusion MRI or perfusion CT to confirm that they had sufficient amounts of salvageable tissue to make surgery viable.
The researchers determined that the best independent predictors of improved functional outcome 90 days after surgery were younger age, lower baseline National Institutes of Health Stroke Scale score, and lower blood glucose level. In addition, they found that the improvements in functional outcome were nearly the same for patients who waited longer for treatment (within the 16-hour window) and for those who underwent CT instead of MRI.
| Perfusion MRI vs. perfusion CT for stroke evaluation | ||
| Perfusion MRI | Perfusion CT | |
| Odds ratio for improved outcome after surgery* | 11.9 | 6.1 |
| Median stroke onset-to-imaging time | 10 hours, 33 minutes | 11 hours, 3 minutes |
Overall, the proportional benefit of endovascular therapy was uniform across patients of various ages regardless of the symptom severity, time to treatment, location of occlusion, and type of perfusion imaging they underwent, the authors noted. Patients benefited from endovascular therapy whether they underwent perfusion CT or perfusion MRI to determine their eligibility for surgery, indicating that either modality could be used for patient selection.
"Endovascular therapy in the 6- to 16-hour time window among patients with evidence of salvageable tissue on brain perfusion imaging is beneficial in a broad patient population, including patients who range in age from 23 to 90 years, who have mild or severe symptoms ... [and] who are selected by CT or MRI," they wrote.