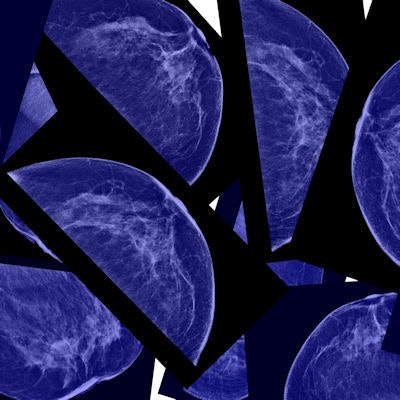
Which is better when it comes to assessing breast tissue density -- man or machine? Turns out radiologists do just fine evaluating dense tissue using BI-RADS measures, compared with the performance of automated software, according to a new study published in the February edition of Radiology.
The findings run contrary to those published in a recent study that suggested automated density measurement tools are the better option, due to their ability to reduce the interreader variability that can occur with BI-RADS assessment. Radiologists assign a BI-RADS density category by visually evaluating the image.
"Gauging density using BI-RADS categories is comparable in accuracy to using computerized tools," corresponding author Dr. Daniel Rubin of Stanford University told AuntMinnie.com.
Discerning density
 Dr. Daniel Rubin of Stanford University.
Dr. Daniel Rubin of Stanford University.Currently, breast density is evaluated by a radiologist using the four-category BI-RADS rating system, Rubin said. But this BI-RADS rating may be hampered by interreader variability, which has prompted the development of automated tools (Radiology, February 2017, Vol. 282:2, pp. 348-355).
"At this point, there are a number of methods for estimating density -- and its utility for estimating the patient's breast cancer risk -- but little clinical literature that has compared them," he said. "So that's what we wanted to do: assess their relative differences and benefits."
Rubin and colleagues compared radiologists' BI-RADS assessments of density with those generated by the University of Toronto's semiautomated Cumulus software and Volpara's VolparaDensity. Cumulus estimates the percentage of breast area that consists of dense tissue, while VolparaDensity produces volumetric measurements of breast density.
The study included 125 women with invasive breast cancer and 274 age- and race-matched control subjects, all of whom underwent digital mammography screening between 2004 and 2013. The researchers then calculated odds ratios and the area under the receiver operating characteristic curve (AUC) for the three modes of assessing density.
Rubin's group found that all three density assessments were positively associated with breast cancer risk (as expressed through odds ratios); however, clinical assessment with BI-RADS showed the best discrimination of patients from control subjects (as expressed through AUC values), though these values were not statistically significant.
| Comparison of BI-RADS, Cumulus, and Volpara density assessments | |||
| BI-RADS | Cumulus (percentage of density) | Volpara (volumetric percentage of density) | |
| Odds ratios of association of density with cancer risk (women with extremely dense tissue compared to those with scattered fibroglandular density) | 2.06 | 2.09 | 2.05 |
| Accuracy of density estimation (AUC) | 0.68 | 0.66 | 0.64 |
What's the bottom line? BI-RADS classification was as accurate as computer-assisted methods of evaluating breast tissue density, the researchers concluded.
Don't throw out the baby
There is definitely a place for automated density assessment, according to Rubin and colleagues. Automated methods offer benefits such as improving the reproducibility of breast density evaluations over time.
"Future development of automated methods to quantify breast density and other risk features could improve risk prediction with full-field digital mammography images," the group wrote.
The study findings support the use of BI-RADS categories as an appropriate tool to measure tissue density and to help estimate a woman's risk of breast cancer. But better methods are needed to allow for more precise risk prediction using breast tissue features, Rubin concluded.
"Current automated quantitative approaches don't necessarily yield more information than BI-RADS assessment," he said. "So radiologists can keep using BI-RADS with confidence."



















