California researchers have found links between the appearance of triple-negative breast cancer on two different imaging modalities, MRI and PET/CT. They believe their findings can help guide therapy for the disease, which occurs less frequently but is typically more deadly than other types of breast cancer, according to a study published online July 22 in Radiology.
Researchers from the University of California, San Francisco (UCSF) found a strong association between dynamic contrast-enhanced (DCE) MRI signal enhancement ratio and maximum standardized uptake values (SUVmax) from PET/CT scans. The relationship could help illustrate the progression of triple-negative breast cancer and be a valuable tool to assess a patient's prognosis, they concluded.
The UCSF team found that as high-washout MRI volume increased by 1%, SUVmax increased by 1.57% in primary invasive breast cancer. In addition, SUVmax rose by 4.34% with each 1% gain in high-washout MRI volume in tumors with the triple-negative phenotype.
"The findings provide additional support that imaging biomarkers, including dynamic contrast-enhanced MR imaging signal enhancement ratio and SUVmax, relate to breast cancer aggressiveness and, therefore, may be valuable for prognostic assessment," lead study author Dr. Marjan Bolouri, from the departments of radiology and biomedical imaging at UCSF, and colleagues wrote.
A particularly deadly cancer
Triple-negative breast cancer accounts for 10% to 20% of all breast cancers, but it causes a relatively large proportion of deaths and has a high rate of distant metastases at diagnosis, the researchers noted.
Because DCE-MRI and FDG-PET/CT can visualize the functional properties of breast tumors, the modalities have increasingly been used to evaluate invasive breast cancer. DCE-MRI, for example, can quantify tumor progression through signal enhancement ratios, while SUVmax as measured by FDG-PET can indicate breast cancer metabolic activity.
In this retrospective study, the researchers examined medical records at UCSF to identify patients with a diagnosis of invasive breast cancer between January 2005 and December 2009. Potential participants received both breast DCE-MRI and whole-body FDG-PET/CT scans within six months before or after their diagnoses. The time between the MRI and PET/CT exams ranged from zero to 72 days, with an average of 7.6 days.
MRI exams were performed on a 1.5-tesla system (Signa, GE Healthcare) or 3-tesla system (Magnetom Verio, Siemens Healthcare) with patients in a prone position with either four- or eight-channel breast coils. The protocol included a contrast injection of 0.1 mmol/kg of gadopentetate dimeglumine (Magnevist, Bayer HealthCare Pharmaceuticals).
FDG-PET/CT examinations were performed on a PET/CT system with a 16-slice CT device (Biograph 16, Siemens) or a 64-slice CT system (Discovery VCT, GE). Patients received 12.5 mCi (± 2.5 mCi) of FDG, with scans starting approximately 60 minutes (± 15 minutes) thereafter.
Patients were also given a 150-mL injection of iohexol (Omnipaque 350, GE) for the CT scans, with PET exams conducted in 3D mode with seven to 10 bed positions immediately after CT.
Image interpretation
Signal enhancement ratio (SER) was calculated by comparing early-to-late signal enhancement on a per-voxel basis. Voxels with SER values between 1.3 and 1.75 and greater than 1.75 displayed high washout and very high washout kinetics, respectively. Voxels with SER values from 0.7 to 1.0 and 1.0 to 1.3 showed low to medium washout kinetics, respectively. Voxels with SER values from 0.0 to 0.7 were deemed as low washout.
For SUV measurement, PET, CT, and fused PET/CT images had a region of interest placed over any FDG-avid breast focus by two radiologists who were blinded to MRI results and patients' pathologies.
Bolouri and colleagues analyzed 117 invasive breast cancers in 117 patients, with an average tumor size of 3.8 cm. Volume, grade, hormone receptor, and human epidermal growth factor receptor 2 (HER2) status were available for 110 tumors (94%), while hormone receptor and HER2 status were available for 115 tumors (98%). Twenty-four lesions (20%) demonstrated the triple-negative phenotype.
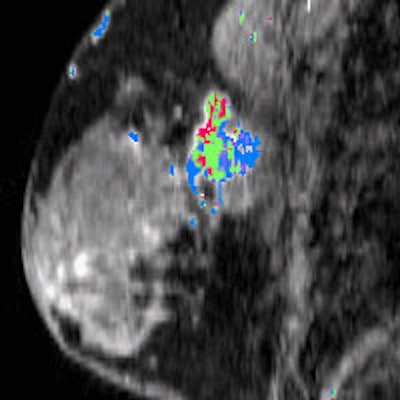
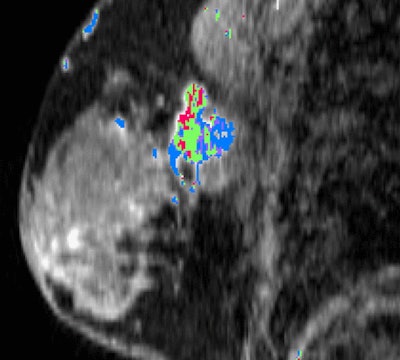 Above: A lesion is found in the upper outer left breast through postgadolinium DCE-MRI with a SER-based color map overlay that shows high washout kinetics (red). Below: A fused contrast-enhanced PET/CT image shows a metabolically active lesion (arrow). Images courtesy of Radiology.
Above: A lesion is found in the upper outer left breast through postgadolinium DCE-MRI with a SER-based color map overlay that shows high washout kinetics (red). Below: A fused contrast-enhanced PET/CT image shows a metabolically active lesion (arrow). Images courtesy of Radiology.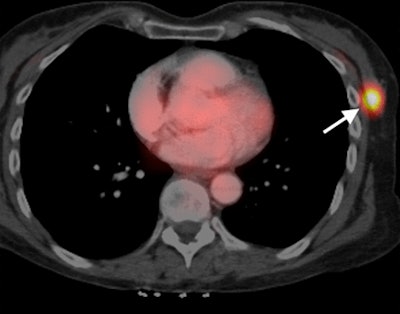
Overall, a greater percentage of high washout was positively associated with SUVmax (1.57% increase in SUVmax per 1% increase in high washout), while a higher percentage of low kinetics was negatively associated with SUVmax (1.2% decrease in SUVmax per 1% increase in low kinetics).
The relationship between the two parameters was greatest among triple-negative tumors (4.34% increase in SUVmax per 1% increase in high washout and 2.65% decrease in SUVmax per 1% increase in low washout).
"Our results showed an association between SER and SUVmax in patients with invasive primary breast cancer who had not undergone treatment, and this relationship is particularly strong among cancers of the triple-negative subtype," the authors concluded.
The correlations were "stronger and more statistically significant," they noted, after adjusting for tumor size, tumor grade, and hormone receptor or HER2 status for both tumors groups.
Bolouri and colleagues suggested that future research might focus on how the concordance between blood flow and glucose metabolism changes after therapy, and how the results might be applied to treatment of triple-negative breast cancer.
As certain subgroups of triple-negative breast cancer demonstrate greater sensitivity to particular therapeutic agents, another area for future investigation could be the identification of the differences in DCE-MRI and PET/CT correlations between subgroups for more targeted chemotherapy.
The authors cited several limitations of the study, including a sample of patients mostly with advanced disease. "Therefore, the ability to generalize our results to the breast cancer population at large is limited," they wrote.
Also, even with a relatively large number of patients with DCE-MRI and PET/CT scans prior to treatment, only 24 cases of triple-negative breast cancer were reviewed.



















