Radiologists reading breast screening studies had comparable performance regardless of whether the images were acquired with computed radiography (CR) or digital radiography (DR) mammography systems, according to a Belgian study published online in European Radiology. Still, DR delivered a lower radiation dose than CR.
Of late, researchers have expressed concern about the performance of CR-based mammography compared to DR. A recent study published by Canadian researchers found that CR was 21% less effective than DR in cancer detection (Radiology, May 14, 2013).
But the Belgian study's results suggest that the worry is unfounded, noted lead author Dr. Hilde Bosmans of University Hospitals Leuven and colleagues.
"Our screening indicators are reassuring for the use of CR and DR," they wrote. "Screening performance parameters for CR and DR technology are not significantly different."
Data that evaluates CR systems in a screening setting are scarce, despite the fact that these devices are widely used in Europe, according to Bosmans' group. To rectify this, the team compared technical and clinical screening performance parameters between the two technologies, including data from 73,008 women screened with CR and 116,945 women screened with DR between 2008 and 2010. Both groups were screened twice (Eur Rad, May 21, 2013).
Clinical indicators assessed by the researchers included recall rate, cancer detection rate, percentage of ductal carcinoma in situ identified, percentage of cancers with T-scores smaller than 1 cm, and positive predictive value. The study found:
- Recall rates for CR and DR in the first round of screening were 5.48% compared with 5.61%; subsequent screening rounds had recall rates of 2.52% and 2.65%.
- Cancer detection rates were 0.52% for CR and 0.53% for DR.
- Rates of ductal carcinoma in situ (DCIS) were 0.08% for CR and 0.11% for DR.
- Rates of cancers with T-scores smaller than 1 cm were 0.11% for both technologies.
- The positive predictive value of CR was 18.45% compared with DR's 18.64%.
None of these parameters showed statistically significant differences between CR and DR technology.
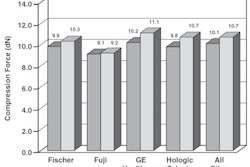
But there was a difference between the two modalities in technical performance, namely, the mean glandular dose (MGD) needed. The study assessed this by measuring the MGD level of routine practice, and found that CR's MGD was 2.16 mGy, compared with DR's 1.35 mGy -- a 60% difference. Although these values still fall under guidelines established in 2006 by the European Council, CR's higher MGD should be taken into consideration, according to Bosmans' team.
"The higher doses used with CR technology versus DR for a screening examination at the age of 50 years could lead to an extra 1.6 radiation-induced cancers per 100,000 women screened," they wrote. "However, the expected benefit of reduction in premature mortality afforded by routine mammographic screening in terms of either lives saved or years of life saved greatly exceeds this risk."