
A new 3D breast imaging technique, stereoscopic digital mammography, has the potential to improve the accuracy of breast cancer screening while also reducing recall rates, according to a study published online November 13 in Radiology.
Researchers at Emory University School of Medicine found that compared to conventional digital mammography, stereoscopic digital mammography boosted specificity by 3.4 percentage points -- and reduced the recall rate by 3.3 percentage points.
Limitations of conventional mammography include missing true focal findings masked in 2D images by normal tissue, and the inability to easily gather information about the volumetric structure of a detected lesion, according to Dr. Carl D'Orsi and colleagues. Stereoscopic digital mammography offers antidotes to these limitations by providing direct, in-depth views of the internal structure of the breast (Radiology, November 13, 2012).
"Stereoscopic digital mammography duplicates how humans already see the world," D'Orsi told AuntMinnie.com. "We wanted to make use of what the human visual system does anyway, and explore whether it would improve mammography."
Masking of true lesions could be reduced with stereoscopic digital mammography because the lesion may be seen as separate from normal tissue, aligned with it but at different depths in the breast volume, according to the team.
"False-positive findings may be reduced with stereoscopic digital mammography, since normal fibroglandular tissue, or isolated elements of calcium, at different depths within the breast will be seen to lie at different depths and, therefore, not superimpose to resemble a lesion," D'Orsi's group wrote.
How does the stereoscopic digital mammography device work? For the study, radiologists read the stereoscopic digital mammography images on a medical stereo display made up of two 5-megapixel grayscale monitors mounted one above the other, with a 110° separation between the two faces. Each stereo image pair was displayed on one of the two monitors. A glass plate with a half-silvered coating was placed between the two monitor faces, bisecting the 110° angle between them, according to the authors.
The image presented on the lower monitor was transmitted through the glass plate, while the image presented on the upper monitor was reflected from the top surface of the glass plate. The radiologists wore passive cross-polarized glasses, so that each eye saw only one of the two images; the radiologists' visual systems then fused the two images into a single, directly visible in-depth image of the breast, D'Orsi and colleagues wrote.
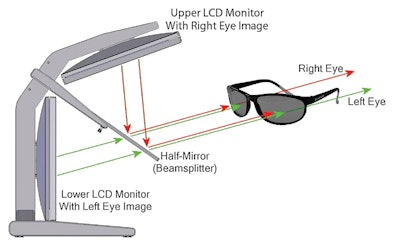 |
| Above, schematic of the stereo display. Below, the complete stereo system used in the study. Images courtesy of RSNA. |
 |
Fewer recalls
The researchers included 1,298 exams acquired between September 2004 and December 2007 from 779 patients; the women underwent both digital mammography and stereoscopic digital mammography examinations in a single visit. Five radiologists participated in the study, and exam findings were interpreted by two radiologists on the same day, without knowledge of each other's reading results.
Compared with digital mammography, stereoscopic digital mammography was more specific (91.2% versus 87.8%, p < 0.0024) and accurate (90.9% versus 87.4%, p < 0.0023) for the detection of breast cancer. Sensitivity did not differ significantly between the modalities (68.4% for stereoscopic digital mammography, compared with 63.2% for digital mammography, p < 0.99). However, stereoscopic digital mammography produced fewer callbacks, with a recall rate of 9.6%, compared with 12.9% for digital mammography.
Dose concerns?
Each of the images in the stereo pairs for the study was acquired with a full standard x-ray dose -- which does raise radiation exposure concerns, D'Orsi and colleagues wrote.
"[For] stereoscopic digital mammography to be acceptable for routine screening, the dose for each image of each pair would have to be halved, so that the combined dose for each stereo view does not exceed the dose of each digital mammography view," the team wrote. "The question then is whether stereoscopic digital mammography with half-dose images comprising each stereo pair would show the same general results."
The researchers are now repeating the study using the same dose as for regular screening mammography, D'Orsi said.
"Now that we know the technique works, we can investigate how low we can drop the dose," he said.
A new niche
Where does stereoscopic digital mammography fit in breast cancer screening, especially because modalities such as digital breast tomosynthesis (DBT) and dedicated breast CT continue to develop?
DBT and dedicated breast CT both produce section-by-section views of the breast volume, and like stereoscopic digital mammography, they are used to overcome the limitations of imaging a 3D structure with a 2D technology -- that is, standard mammography. But neither of these modalities can provide a direct visual depiction of the volumetric structure of the breast, according to D'Orsi's team.
"There are two potentially complementary roles of stereoscopic [digital mammography] and tomographic imaging," the group wrote. "First, as hardware for tomosynthesis advances, it will provide platforms ideally suited for rapid acquisition of stereo image pairs because of the automated x-ray tube movement already installed in the system. Second, there is the possibility of providing the radiologist with stereo projections through all or a portion of the stack of reconstructed tomographic sections, all without any dose penalty."



















