New research has raised serious concerns about the accuracy of chest x-ray interpretations in acute care by nonradiologists and highlighted the urgent need for better training in this area.
A group from Tehran, Iran, examined nonradiologist proficiency for diagnosing acute pathologies on chest x-ray and found that interpretations were "suboptimal" in a large number of cases. When pathologies are acute, an incorrect interpretation often can have an effect on patient mismanagement and a severe impact on outcome, and the authors suggest action must be taken to improve both nonspecialist interpretation and access to radiological expertise.
 Dr. Ghazaleh Mehdipoor from Tehran, Iran.
Dr. Ghazaleh Mehdipoor from Tehran, Iran."Prior studies from various countries ... showed suboptimal knowledge and experience among nonradiologists," lead author Dr. Ghazaleh Mehdipoor, a recent medical graduate from Shahid Beheshti University of Medical Sciences, told AuntMinnieEurope.com. "Much less is known about how nonradiologists interpret common acute cardiopulmonary pathologies such as pulmonary edema or pneumothorax so we decided to evaluate this issue. Most of our participants failed to correctly diagnose the majority of acute pathologies and further, many of them misread the normal chest x-rays as being abnormal."
In the study, published online in BMC Medical Imaging on 18 August, the researchers used a prospective electronic survey to measure the interpretation accuracy of two subsets of nonradiologists: 67 senior medical students and 33 general practitioners (GPs).
The survey included nine hypothetical clinical vignettes, each associated with a chest x-ray that showed only a single acute chest pathology. For example, a vignette for a patient with dyspnea and pleuritic chest pain contained a classic image of pneumothorax. The researchers further added a low-risk vignette associated with a normal chest x-ray. They asked participants to read each of the 10 vignettes, look at the chest x-rays, and type in the pathology they believed they saw. Also, they asked them to state their confidence in the diagnosis and indicate any prior exposure to the topics.
The mean score was 3.57 correct diagnoses out of 10. The self-reported exposure to a similar chest x-ray in the "normal" vignette was 44% of participants.
The survey, conducted between 20 January and 20 February 2015, was distributed to senior medical students in their seventh year, all of whom had trained in radiology during clinical rotations, and GPs in Tehran. Participants had to free text the name of each pathology or select "normal" or "I don't know." Each correct diagnosis per vignette scored 1, and each incorrect answer scored 0. This led to a sum score of 0 to 10 for the entire survey for each participant.
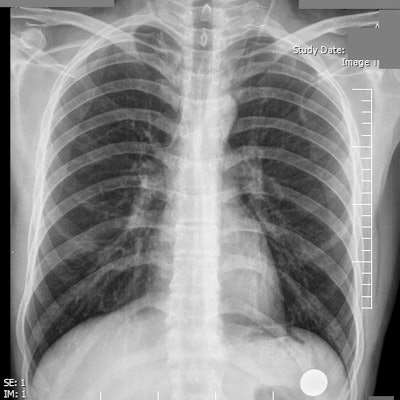
 Top: A patient complains of intermittent dyspnea and chest pain. Only 15% of survey participants correctly indicated a normal chest x-ray, and just 44% of study participants claimed prior exposure to a similar image. Image courtesy of Shahid Beheshti University of Medical Sciences. Bottom: A 65-year-old man with a remote history of myocardial infarction presents with worsening dyspnea, shortness of breath, and progressive respiratory distress. The chest x-ray demonstrates bilateral pulmonary hilar vascular engorgement, resulting in "bat's wing" appearance accompanied by less perceptible prominence of pulmonary vascular markings through the peripheral zones and presence of cardiomegaly. The diagnosis is acute pulmonary edema. Available at chestatlas.com. Reproduced with permission from Chest Atlas.
Top: A patient complains of intermittent dyspnea and chest pain. Only 15% of survey participants correctly indicated a normal chest x-ray, and just 44% of study participants claimed prior exposure to a similar image. Image courtesy of Shahid Beheshti University of Medical Sciences. Bottom: A 65-year-old man with a remote history of myocardial infarction presents with worsening dyspnea, shortness of breath, and progressive respiratory distress. The chest x-ray demonstrates bilateral pulmonary hilar vascular engorgement, resulting in "bat's wing" appearance accompanied by less perceptible prominence of pulmonary vascular markings through the peripheral zones and presence of cardiomegaly. The diagnosis is acute pulmonary edema. Available at chestatlas.com. Reproduced with permission from Chest Atlas.Confidence in the diagnosis was measured on a five-point Likert scale, with greater certainty reflected by a higher score. Exposure to the pathology was indicated through a yes/no option. Three radiologists and six medical students piloted the survey, with the radiologists scoring 100% for the vignette diagnoses.
The overall mean score achieved by all participants was 3.57. In the subsets, the medical students' mean score was 3.77, while GPs' mean score was 3.15. No significant difference was measured between the two scores (p = 0.15). The maximum score in both groups was 8 out of 10, and only eight participants correctly diagnosed more than seven vignettes.
Overall, the highest rate of correct diagnosis was for diaphragmatic herniation (77%), followed by pneumoperitoneum (67%) and pneumothorax (54%). The lowest rate of correct diagnosis occurred for acute respiratory distress syndrome (ARDS) (8%), foreign body (12%), and the low-risk vignette associated with the normal chest x-ray (15%). The key findings are shown on the table below.
| Percentage of correct diagnoses for acute chest pathologies | |||
| Correct (%) | Correct and certain (%) | Prior exposure (%) | |
| Pulmonary edema | 40 | 31 | 45 |
| Pericardial effusion | 27 | 19 | 62 |
| Aortic dissection | 24 | 22 | 13 |
| Normal | 15 | 13 | 44 |
| Pneumothorax | 54 | 19 | 54 |
| Tension pneumothorax | 33 | 18 | 45 |
| Pneumoperitoneum | 67 | 23 | 68 |
| Diaphragmatic herniation | 77 | 50 | 31 |
| Foreign body | 12 | 9 | 30 |
| ARDS | 8 | 7 | 22 |
Furthermore, participants indicated greatest certainty (Likert scale: 5) for pneumoperitoneum (46.9% of participants) and pneumothorax (41.8%), while the greatest degree of uncertainty (Likert scale: 1) belonged to ARDS (24.7%) and foreign body (19.3%). Self-reported certainty in the diagnosis was associated with the correctness of diagnosis for only pneumoperitoneum (p < 0.001), tension pneumothorax (p < 0.001), and pulmonary edema (p < 0.05), but not for the other conditions.
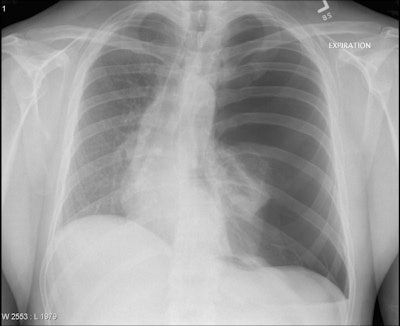 A 29-year-old man presents with severe respiratory distress and hypotension in the setting of persistent left hemithorax pain following a cough attack. The chest x-ray demonstrates loss of pulmonary vascular markings on the left side, leading to its remarkable left hemithoracic translucency associated with left pulmonary total collapse and rightward mediastinal shift. The diagnosis is tension pneumothorax. Available at chestatlas.com. Reproduced with permission from Chest Atlas.
A 29-year-old man presents with severe respiratory distress and hypotension in the setting of persistent left hemithorax pain following a cough attack. The chest x-ray demonstrates loss of pulmonary vascular markings on the left side, leading to its remarkable left hemithoracic translucency associated with left pulmonary total collapse and rightward mediastinal shift. The diagnosis is tension pneumothorax. Available at chestatlas.com. Reproduced with permission from Chest Atlas.Participants also indicated prior exposure most commonly for pneumoperitoneum (68%) and pneumothorax (54%), which corresponded to two of the most correctly diagnosed vignettes. However, less than half of the participants (44%) claimed to have seen a similar image to the normal chest x-ray. The researchers found an association between self-reported exposure to similar images and the correctness of diagnosis for pneumoperitoneum, pericardial effusion, and pulmonary edema (p < 0.05 for all), but not for the rest.
Significant deficiencies
Most participants failed to diagnose the majority of acute pathologies with diagnostic clues on chest x-ray, according to the researchers. Furthermore, the vast majority (85%) had trouble identifying the normal chest x-ray as being normal, with less than half reporting to have seen it before. Significant knowledge deficiency was deemed to be the main source of errors.
"Surprisingly, many participants reported to have been certain of a diagnosis when their designated diagnosis was, in fact, incorrect; which could ultimately impact clinical decision-making. Only 59% had appropriate self-perception about the correctness or incorrectness of their answers, as reflected by their self-reported certainty in their answers," they wrote.
A key limitation of the study was it tested diagnostic capacity for one pathology at a time, whereas in real practice patients often presented with more than one condition or disease visible on chest x-ray and with vaguer scenarios and history than the classic scenarios that were presented in the vignettes. However, this suggested that in real life, correct interpretation by nonradiologists would be even lower, according to the group.
Mehdipoor believes that while the magnitude of deficiency might vary between centers, suboptimal interpretation among nonradiologists is a widespread problem occurring around the world and that practitioners' false perception of a correct diagnosis could ultimately endanger patients' health. The study findings, therefore, should be of importance to policymakers, she added.
"The educational curricula for students and continuous medical education for practitioners should focus more on teaching them to distinguish between abnormal and normal chest x-rays and diagnose acute, particularly life-threatening, pathologies and common diseases," she said. "As an interim measure, the use of secure platforms and apps to permit the sharing of cardiopulmonary chest x-rays for teleconsultation might be a practical solution when onsite radiologists aren't available."
Mehdipoor hopes to follow up the research with additional studies and is planning a second survey of the same participants to see if they perform differently after a period of time spent improving their chest x-ray interpretative knowledge. She is also exploring the possibility of running the survey in other countries.



















