Apparent diffusion coefficient (ADC) values generated by MRI scans may be a promising tool to monitor early response and predict prognosis after chemotherapy for non-small cell lung cancer (NSCLC), according to a study published online August 18 in Radiology.
Researchers from Japan concluded that patients with advanced NSCLC could avoid the cost and unnecessary harm of ineffective chemotherapy and receive more effective treatment sooner, if initial chemotherapy is found to be ineffective based on early ADC changes.
"If physicians could detect an early response to chemotherapy on the basis of results of an imaging modality, patients could switch anticancer drugs after the first cycle of chemotherapy if the drugs have proved ineffective," wrote lead study author Dr. Hidetake Yabuuchi, PhD, from the department of clinical radiology at Kyushu University, and colleagues.
ADC research
CT scans are often performed on NSCLC patients after two rounds of chemotherapy to assess treatment efficacy, according to the authors. Other modalities have been explored for treatment monitoring, such as dynamic contrast MRI, FDG-PET, and perfusion CT. The authors believe that frequently evaluating patients with PET and CT can increase radiation doses for patients, so they decided to investigate the efficacy of MRI instead.
Past studies have shown that ADC values from diffusion-weighted MRI can be useful in predicting and detecting a response to chemotherapy or chemotherapy and radiation therapy early in various malignant tumors, Yabuuchi and colleagues added.
The prospective study recruited 28 patients (17 women, 11 men) with a mean age of 64.8 years from April 2008 to March 2010. The subjects had histologically confirmed stage IIIB or IV advanced NSCLC. There were 22 cases of adenocarcinomas, five squamous cell carcinomas, and one large cell carcinoma.
The study excluded patients with renal dysfunction or an allergy to the contrast agent gadopentetate dimeglumine (Magnevist, Bayer HealthCare Pharmaceuticals), as well as those who planned to undergo chemotherapy and radiation therapy for primary lung cancer, patients whose treatment was interrupted after one round of chemotherapy due to the progression of the disease, and cases where the tumor could not be adequately visualized on MRI.
All 28 patients received chemotherapy and underwent 1.5-tesla MRI (Achieva, Philips Healthcare) within one week prior to the first course of chemotherapy and again three to four weeks after the start of the first course of chemotherapy.
NSCLC progression
To determine the change in tumor size after two courses of chemotherapy, the researchers also performed a pretreatment chest CT scan on patients within one week prior to the first round of chemotherapy, with a follow-up CT scan after two courses of chemotherapy six to eight weeks after the start of chemotherapy.
The maximum diameter of the target lesions on pretreatment CT images ranged from 23 to 90 mm, with a mean size of 47.3 mm. Diffusion-weighted MRI was performed for three sections, including the maximum diameter section, with ADC maps generated from the diffusion-weighted images.
Dynamic contrast-enhanced MR images with gadopentetate dimeglumine administered intravenously based on body weight were acquired sequentially before and after contrast material injection.
For MR image analysis, one study co-author manually placed regions of interest within a given lesion to determine ADC values. Another co-author analyzed both pretreatment and post-treatment CT images.
During and after chemotherapy treatment, patients were monitored with clinical evaluations at regular intervals, in addition to undergoing chest CT, radiography, and other imaging studies as clinically indicated. The median follow-up time was 12.8 months, ranging from 2.2 to 31.2 months.
'Significant correlation'
The final analysis of data showed a "significant correlation" between early ADC change and tumor size reduction rate after two courses of chemotherapy. The early ADC value change before therapy and after one course of chemotherapy ranged from -13.5% to 49.5%, with a median change of 26%.
The researchers further divided patients who underwent diffusion-weighted MR imaging and dynamic contrast-enhanced MR imaging into two groups according to the changes in ADC. One group included patients with an ADC increase equal to or greater than the median ADC change (good ADC increase), while the other group had an ADC increase less than the median ADC change (poor ADC increase).
The mean early ADC change was 35.9% in the group of 15 patients with good ADC increase, compared with an early ADC change of 7.1% in the group of 13 patients with poor ADC increase.
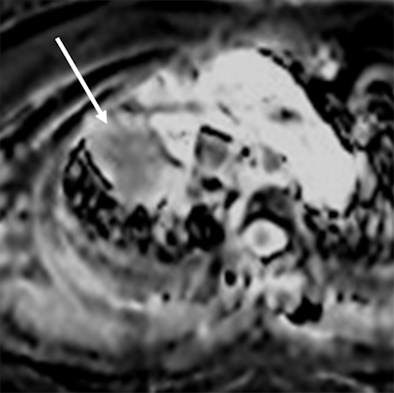 |
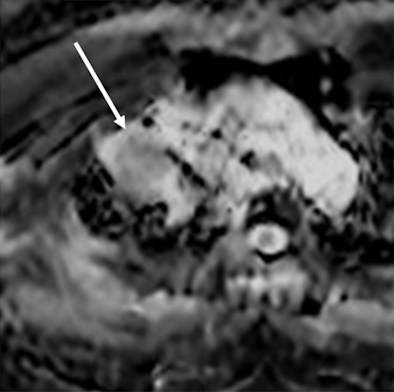
| MR images of a 75-year-old woman with lung cancer who achieved a partial response after two rounds of chemotherapy. ADC maps obtained before (above) and after (below) one course of treatment indicate that the ADC value of the lesion (arrow) increased from 0.99 to 1.48 x 10-3 mm2/sec after therapy. Images courtesy of Radiology. |
 |
The median progression-free survival for the group with good ADC increase was 12.1 months, compared with 6.7 months for the group with poor ADC increase. In addition, the median overall survival period was 22.4 for the good ADC increase group, compared with 12.3 months for the poor ADC increase group.
"Our study results indicate that early response to and prognosis after chemotherapy in patients with NSCLC could be detected in terms of ADC change but not in hemodynamic or morphologic changes at MR imaging," Yabuuchi and colleagues concluded.
The authors noted several limitations of the study, including a relatively small patient sample and the fact that the chemotherapy regimens did not include molecular-target or antiangiogenic agents.
"It is important to evaluate whether early ADC change can predict early response better than hemodynamic change at MR imaging in patients who receive molecular-target or antiangiogenic agents," they wrote.