Mining new ore from their groundbreaking VC study data of 2003, Drs. Perry Pickhardt, Richard Choi, and colleagues have published two more studies based on the data from the multicenter trial of 1,233 asymptomatic patients who underwent virtual and conventional colonoscopy.
The original study, the first to conclude that VC could slightly outperform conventional colonoscopy in average-risk patients, was hailed as a bright new chapter in colorectal cancer screening following its publication in the New England Journal of Medicine (December 4, 2003, Vol. 349:23, pp. 2191-2200).
The new studies, based on the same group of 728 men and 505 women ages 40-79 (mean age 57.8 years), are eye-opening in their own right. The first, in the September 7 issue of Annals of Internal Medicine, examines the adenoma miss rate of virtual colonoscopy -- not compared with an imperfect conventional colonoscopy gold standard, but on its own -- as well as the miss rate of the conventional exam.
The authors concluded that conventional colonoscopy has significant blind spots in which VC can excel -- both clinically, in terms of polyp detection, and statistically, once the burden of an imperfect conventional colonoscopy gold standard has been lifted. As a result, they recommended adding virtual colonoscopy as a front-line colorectal cancer screening exam.
The above-average VC results depend heavily on the good training of the participating radiologists, as well as on the group's use of an advanced 3D interpretation system, they stated.
The second study, in September's Radiology, examines the size, prevalence, and distribution of nonadenomatous polyps from the same study cohort. VC is more likely to detect an adenomatous polyp than a nonadenomatous polyp of the same size, the authors found.
The results are based on data from 1,233 subjects at three centers who underwent same-day screening and conventional colonoscopy in 2002 and 2003. Candidates with signs of rectal bleeding and a history of prior polyps or cancer were excluded, as well as those who had colorectal cancer screening exams in the previous 10 years. Following purgative cleansing with a double-dose phosphosoda prep and 10 mg of bisacodyl, and a 2.1% barium oral contrast agent to mark fecal residue, the patients were insufflated manually with room air.
CT images were obtained on either a four- or eight-slice multidetector-row scanner using 2.5-mm or 1.25-mm collimation, respectively. Both prone and supine scans were performed using 15 mm/sec table speed, 1-mm reconstruction intervals, 100 mAs, and 120 kVp. Six radiologists trained in virtual colonoscopy used a V3D-Colon workstation (Viatronix, Stony Brook, NY) for primary 3D interpretation, reserving 2D for problem-solving and correlation of all positive results. The conventional colonoscopy results were segmentally unblinded, allowing for the assessment of any false-negatives in conventional colonoscopy, which served as the reference standard.
VC sets its own standard
Previously reported estimates of adenoma miss rates at conventional colonoscopy have relied on repeated examination with the same exam, the authors wrote in the Annals of Internal Medicine. Most adenomas detected at follow-up surveillance are believed to have been missed at the initial exam.
"The fact that OC (optical, or conventional colonoscopy) has been the reference standard to determine its own miss rates is a major drawback, largely because systematic errors from certain 'blind spots' (such as behind haustral folds) can go undetected on repeated examination," they wrote (Annals of Internal Medicine, September 7, 2004, Vol. 141:5, pp. 1-9).
By this standard, of course, VC-detected polyps that OC doesn't detect are routinely written off as false-positives in VC, even though a certain number represent lesions missed at OC. Therefore, in an effort to better assess virtual colonoscopy's true performance, the segmental unblinding technique used in the original series was tapped to assess colonoscopy's performance, as well as that of virtual colonoscopy.
"An in-depth analysis of the VC miss rate ... is beyond the scope of this paper," they acknowledged. "Nonetheless, VC and OC represent complementary techniques for polyp detection, since all known misses by one study are necessarily detected by the other."
Segmental unblinding
In OC, one of 17 experienced colonoscopists measured each polyp using a calibrated linear probe (the polyp-matching algorithm requires agreement according to size and location). After evaluation of each colonic segment in OC, VC results were unblinded, and anytime polyps were seen on VC but not OC, the colonoscopist closely re-examined the segment. All retrieved polyps were sent for histologic examination.
"Prospective OC performance was compared against the enhanced reference standard of second-look OC after segmental unblinding of VC results," they wrote. OC miss rates were calculated using a chi-square test among the three medical centers, and 95% confidence indices (CIs) were also calculated.
In all, the researchers identified 1,310 polyps, of which 511 (39%) were 5 mm or larger. Of these 511 lesions, 55 (10.8%) were seen only on second-look OC after segmental unblinding of the virtual colonoscopy results for the particular segment. Of the 55 lesions OC found after unblinding, 24 (43.6%) were nonadenomatous (including 16 hyperplastic polyps), leaving 31 missed neoplasms. Of these 31, 10 5-mm polyps were excluded from further analysis due to their small size.
In 20/1,233 patients (1.6%), 21 adenomas 6 mm or larger were seen in OC only after VC results were unblinded, representing 20/168 (11.9%) of all patients with adenomas 6 mm and larger.
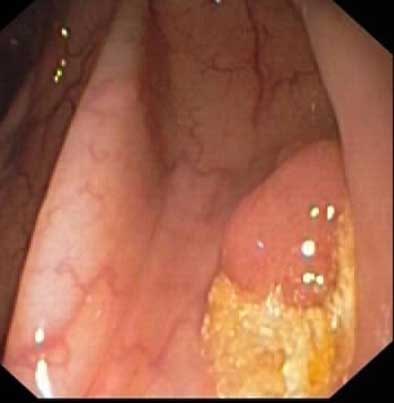 |
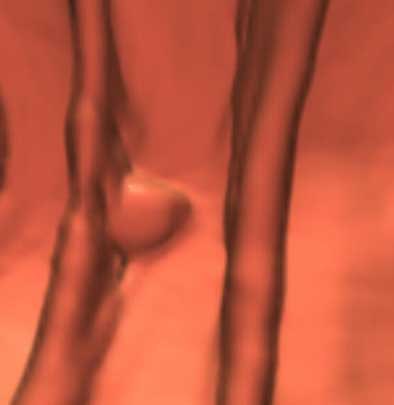
| Above, a 10-mm adenoma behind a fold in the ascending colon was missed prospectively at optical colonoscopy, but found with second-look colonoscopy after initial virtual colonoscopy results showing the polyp (below) were unblinded and the segment re-examined. Images courtesy of Dr. Perry Pickhardt. |
 |
"At 8-mm and 10-mm thresholds, the OC adenoma miss rates by polyp were 10.5% (CI, 5.2% to 18.5%) (10 of 95 adenomas) and 11.8% (CI, 4.4% to 23.9%) (six of 51 adenomas), respectively," the authors wrote. "The 10 patients with missed adenomas 8 mm or greater represented 12.2% (10 of 82 patients) of all patients with neoplasms of this size or greater; the six patients with missed adenomas 8 mm or greater represented 12.5% of all patients with neoplasms 10 mm or greater."
As for histology, 17/21 (81%) of the unblinded neoplasms 6 mm or larger were tubular adenomas, three (14.3%) were tubulovillous adenomas, and one (4.8%) was an adenocarcinoma located proximal to the rectum and not associated with a haustral fold.
In all, 7/21 (33%) of the 21 unblinded polyps were advanced lesions, including those larger than 10 mm with high-grade dysplasia, a prominent villous component, or focus of malignancy. The locations of the 21 lesions missed on first-pass OC were proximal colon, 10 (47.6%), while 6/11 distal lesions were located in the rectum. Fourteen of 15 (93%) of nonrectal missed lesions were located on a fold, 10 of which were located on a proximal aspect, four on a distal aspect, and two on the edge of a fold.
"(Virtual colonoscopy's) adenoma miss rates in our trial were 14.3% (30 of 210 adenomas), 7.4% (7 of 95 adenomas), and 7.8% (four of 51 adenomas) at 6-mm, 8-mm, and 10-mm thresholds, respectively," Pickhardt and colleagues wrote.
A retrospective review of the CT data relating to the 19/21 missed lesions showed that 90.5% could be seen retrospectively in both supine and prone images, while one lesion each could be seen only in supine or prone. At OC the colonoscope reached the cecum in 1,233/1,241 patients, for a high 99.4% completion rate the authors believe spoke to the skill of the endoscopists performing the OC exam. In addition, the colonoscopists knew their answers were being recorded, which may have encouraged them to work carefully, the authors wrote.
"Our findings underscore the enormous potential benefit of adding VC to the front-line screening armamentarium," they stated. "In actual clinical practice, the positive results of a screening VC examination would, of course, not be blinded at subsequent therapeutic OC. Therefore, the colonoscopist would have a prior knowledge of polyp size, morphology, and specific location at VC. In this setting, the overall sensitivity for detecting adenomas would be expected to increase over OC alone."
The results also point out potential trouble spots for conventional colonoscopy -- at the proximal side of folds, the inner aspect of flexures, and the distal rectum, relating in no small measure to the unidirectional nature of the OC exam, they stated. "Meticulous maneuvers and technical advances to physically flatten folds must be balanced with the need for an efficient (OC) examination," they added.
The group concluded that OC is a sensitive diagnostic tool, but even experienced colonoscopists will occasionally miss significant lesions. "By using VC as a separate standard of reference, our study confirms that distinct locations on OC examination represent relative blind spots where clinically significant polyps can sometimes be missed," they wrote. "These findings are an important reminder for colonoscopists, and indicate the need for continued improvements in colonoscopic technology."
Polyp prevalence in an average-risk population
In the Radiology study, based again on the original data but relying this time on OC as the reference standard, Drs. Pickhardt and Choi, along with Drs. Ink Hwang and William Schindler from the University of Wisconsin Medical School in Madison, WI, investigated the prevalence and size distribution of adenomatous and nonadenomatous polyps (Radiology, September 2004, Vol. 232:3, pp. 784-790).
All the lesions removed at OC were analyzed histologically. According to the group's results, 750 (57.7%) polyps identified at OC were nonadenomatous, 622 (82.3%) measuring 5 mm or smaller. The nonadenomatous polyps comprised 64.4% (622/966) of all diminutive lesions, and 39.9% (134/344) of polyps 6 mm and larger (p<0.001).
"The prevalence rate for nonadenomatous polyps was 8.8% (109 of 1,233 patients) and 2.0% (25 of 1,233 patients) at 6- and 10-mm thresholds, respectively," they wrote. "CT colonography by-polyp sensitivity for nonadenomatous lesions was 73.1% (98 of 134 patients) and 73.3% (22 of 30 patients) at 6- and 10-mm thresholds, respectively, compared with 85.7% (180 of 210 patients) and 92.2% (47 of 51 patients) for adenomas (p<0.01)."
The results showed that more than 80% of all nonadenomatous polyps were 5 mm or smaller, and that nonadenomatous polyps still accounted for almost 40% of polyps 6 mm and larger, they wrote.
Small lesions accounted for a more than 80% of nonadenomatous polyps, they wrote, and there is growing consensus that these lesions are of scant clinical significance. Nonadenomatous lesions outnumbered adenomas by 756 to 554 among the average-risk subjects, whereas in previous studies of higher-risk populations, nonadenomatous lesions comprised just 31% to 43% of all polyps, the group wrote.
This study, as well as previous research by Yee et al and Fenlon et al, suggests that given the same polyp size, VC is somehow more sensitive for the detection of adenomatous polyps than it is for nonadenomatous lesions, suggesting that even beyond strict size thresholds, the lesions VC misses may be clinically less important than the ones VC finds.
"This fortuitous decrease in CT colonography sensitivity for nonadenomatous polyps compared with adenomas has received relatively little attention," the authors wrote. "One potential explanation ... is the tendency of hyperplastic polyps to efface or flatten out with air distension of the colon. It is likely that polyp morphology itself plays a role. In our experience, larger nonadenomatous lesions demonstrate an atypical appearance, such as an elongated or flattened shape that exaggerates polyp size relative to polyp volume, more often than do adenomas."
By Eric Barnes
AuntMinnie.com staff writer
September 8, 2004
Related Reading
Virtual colonoscopy shows promise, experts say, September 2, 2004
What virtual colonoscopy misses might not matter, August 18, 2004
Group credits 3-D reading for best-ever VC results, October 15, 2003
Multiobserver performance trial assesses utility of screening VC, November 27, 2002
Copyright © 2004 AuntMinnie.com