VANCOUVER, BC - PET/CT can evaluate lung inflammation and monitor treatment effects in patients with post-COVID-19 lung disease, according to research presented at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting.
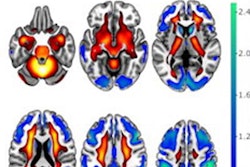
A group in Lucknow, India, performed F-18 FDG PET/CT scans in patients with post-COVID lung disease before and after steroids and antifibrotic drugs treatment. They noted significant decreases in the number, size, and metabolic activity of the lung lesion in the follow-up scans.
"F-18 FDG PET/CT can thus help in evaluating [post-COVID lung disease] inflammatory process, monitor treatment effects, and may help to strategize patient management," said presenter Dr. Yogita Khandelwal, a graduate student at the Sanjay Gandhi Postgraduate Institute of Medical Sciences.
Ongoing respiratory complications are common in patients infected with severe COVID-19. Estimates suggest one-third of patients hospitalized with COVID-19 are affected by respiratory symptoms, with many requiring supplemental oxygen even after testing negative for the virus.
In this study, Khandelwal and colleagues recruited 25 patients with shortness of breath (dyspnea) after COVID-19 infection but who were negative after reverse transcription polymerase chain reaction (RT-PCR) tests. Fourteen had dyspnea on a six-minute walk test at the time of the baseline scan, while 11 patients had dyspnea even at rest. Thirteen patients had persistent oxygen requirements, Khandelwal said.
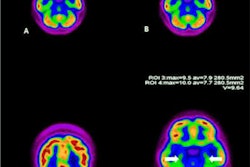
All patients showed metabolically active lesions in both lungs with FDG standard uptake values (SUV) between 2.0 and 12.7 (mean SUVmax of 4.2) and metabolically active mediastinal lymph nodes (mean SUVmax of 3.5, range 2.4-5.1) were noted in 13 (52%) patients, as well as significant CT lung findings.
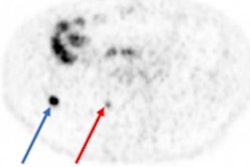
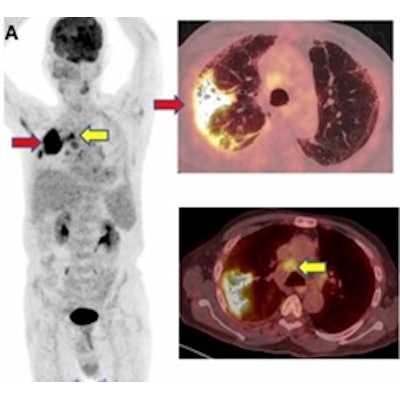
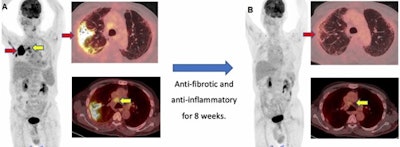 A 71-year-old male diagnosed with COVID-19 in October 2020. After treatment, he was discharged from the hospital. He was readmitted to the hospital for respiratory failure in January 2021 and underwent F-18 FDG PET/CT. (A) Maximum intensity projection whole-body image and axial fused PET/CT show FDG-avid (SUVmax, 12.7) consolidation in the right lung (red arrow). Non-tracer-avid changes are noted in both lungs on CT. FDG-avid mediastinal lymph nodes (SUVmax, 4.4) (yellow arrow) were also noted. The patient was given steroids and pirfenidone for two months. He showed significant improvement in symptoms with no oxygen requirement. (B) Follow-up PET/CT reveals complete resolution of the lung lesion and non-avid residual fibrotic changes in both lungs (red arrow). Mediastinal lymph nodes also show a decrease in avidity (SUVmax, 2.5). Image courtesy of Yogita Khandelwal.
A 71-year-old male diagnosed with COVID-19 in October 2020. After treatment, he was discharged from the hospital. He was readmitted to the hospital for respiratory failure in January 2021 and underwent F-18 FDG PET/CT. (A) Maximum intensity projection whole-body image and axial fused PET/CT show FDG-avid (SUVmax, 12.7) consolidation in the right lung (red arrow). Non-tracer-avid changes are noted in both lungs on CT. FDG-avid mediastinal lymph nodes (SUVmax, 4.4) (yellow arrow) were also noted. The patient was given steroids and pirfenidone for two months. He showed significant improvement in symptoms with no oxygen requirement. (B) Follow-up PET/CT reveals complete resolution of the lung lesion and non-avid residual fibrotic changes in both lungs (red arrow). Mediastinal lymph nodes also show a decrease in avidity (SUVmax, 2.5). Image courtesy of Yogita Khandelwal.Patients received methylprednisolone (a steroid) and pirfenidone (an antifibrotic drug), then underwent a follow-up scan between six and 12 weeks later to evaluate their response to treatment and assess residual lung damage.
Three patients died during the follow-up period due to respiratory septic shock, Khandelwal said. Among the 22 other patients, there was a significant decrease in the number, size, and "FDG avidity" of the previously seen lung lesions, he said.
Specifically, seven (32%) of these 22 patients were found to have active metabolic lesions in the lung parenchyma, with mean SUVmax dropping from 4.2 to 2.7. Also, five (23%) patients showed a mean SUVmax in metabolically active mediastinal lymph nodes dropping from 3.5 to 3.2.
In addition, 16 of 22 patients demonstrated a mixed pattern of residual lung changes on CT. In these 16 patients, CT features included residual mild ground glass opacity (n = 12), fibroreticular changes (n = 4), nodular opacities (n= 2), and fibrotic bands (n = 7), with more than one feature in some.
"F-18 FDG PET/CT proved to be a sensitive tool for monitoring ongoing inflammation and its management," Khandelwal said.
Ultimately, during the pandemic, there was no standard modality to assess residual lung inflammation, and it was difficult to gauge the extent and severity of disease even in recovering patients, Khandelwal noted. Hence, it was challenging to start appropriate treatment.
"Molecular markers identified by F-18 FDG PET/CT can reveal the triggers and sustenance mechanism of inflammation," he concluded. "In the future, this could contribute to the development of new drugs and better management strategies."