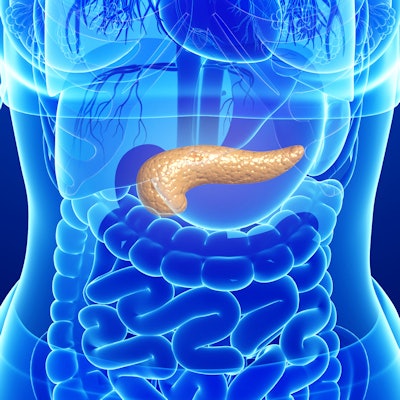
What's the best way to handle cysts detected in the pancreas on imaging exams? Such lesions are relatively common, but only a small number are malignant, so figuring out suitable management surveillance can be a challenge.
How to handle pancreatic cysts was the subject of a keynote address by Dr. Frank Miller at the annual meeting of the Canadian Association of Radiologists April 6-10. Miller is chief of body imaging in the department of radiology at the Feinberg School of Medicine at Northwestern University in Chicago.
"We are not sure if screening all patients with pancreatic cysts will prove efficacious given the large number of patients with cysts and the small percentage of cysts that develop into cancer," Miller said. "We aren't sure what to do with them.
Most cysts are benign
Miller noted that the vast majority of pancreatic cysts are benign.
"We see them in approximately 10% of the population and in up to 30% in those over the age of 70 years old," he said.
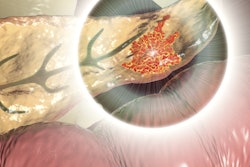
Some of the features to be on the lookout for in terms of concerns about malignancy include the size of the lesion, the number and size of cysts, enhancing modules, an internal enhancing solid component, a thick enhancing wall suggestive of a neuroendocrine tumor or adenocarcinoma (unlike branch-duct intraductal papillary mucinous neoplasia or IPMN, where there is not an enhancing wall), and complexity in the MR image including hemorrhage, nodules, and septa. In addition, clinicians need to watch for dilatation of the main pancreatic duct.
An example of a lesion that a radiologist can diagnose based on appearance, which can often be followed and not biopsied nor resected, is a serous cystadenoma, noted Miller. In contrast, a lesion that should be resected is a mucinous cystic neoplasm, which can mimic a pseudocyst.
"You generally resect these because they have a malignant potential," Miller said, noting that the risk factors for malignancy include advanced age, tumor size of more than 4 cm, and cyst wall irregularity and thickening.
Radiologists can distinguish between mucinous cystadenoma and serous cystadenoma in several ways, Miller noted. One of the ways is advanced age, as serous cystadenomas occur in women of advanced age.
Smaller size is another as serous cystadenomas tend to feature cysts that are less than 1 cm. In contrast, mucinous cystadenomas should be surgically removed because of the possibility of malignancy, according to Miller.
Another lesion that necessitates prompt surgical management is a cystic pancreatic neuroendocrine tumor, Miller noted.
"The presence of a thick enhancing wall raises suspicion for a pancreatic neuroendocrine tumor," he said.
Clinicians need to avoid confusing pancreatic lipomas, which are more common than generally considered, with adenocarcinomas or cystic pancreatic tumors, Miller said.
"It's often not suspected or diagnosed correctly as a lipoma because the fat is not recognized on CT or MR," he said.
Some guidance that Miller offered with respect to managing cystic masses is to consider etiology. If they occur in patients with pancreatitis, they are more likely walled-off necrosis or pseudocysts, whereas if they occur in a patient without pancreatitis, other etiologies should be considered, such as mucinous cystic neoplasm.
One of the more common lesions seen on imaging is intraductal papillary mucinous neoplasms, which currently represent about 20% to 30% of cystic lesions.
"They are asymptomatic and are more common than pseudocysts," he said.
With respect to malignant potential, it is difficult to predict which IPMNs will become malignant, as benign and malignant IPMNs look very similar, Miller said.
"We need to better define the extent of follow-up needed for IPMNs based on clinical and imaging features and other features," Miller said. "Otherwise, I'm afraid we may bankrupt our healthcare system."
Differentiating between main duct IPMNs and branch duct IPMNs is important as the former, while less common, have greater potential for malignancy.
"Invasive cancer develops in as many as 31% to 45.5% (of main duct IPMNs)," he said.
Some imaging modalities, namely endoscopic ultrasound (EUS), may be preferable to identify enhancing nodules in IPMNs, for they may present in a subtle manner, Miller explained.
"EUS shows the nodule best, and the main advantage is you can do a biopsy if needed," he said.
Chief to keep in mind is the field defect, which refers to patients with IPMNs being prone to pancreatic cancer elsewhere in the pancreas, separate from cysts, according to Miller.
Surveillance is an issue
Surveillance of lesions of the pancreas is an issue that is debated, Miller said. Guidelines such as those issued by the American Gastroenterological Association call for discontinuation of radiographic surveillance after five years for patients with stable pancreatic cysts. A paper published in Annals of Surgery in 2017 called into question that recommendation, noted Miller.
"This basically looked at 3,024 patients from a single institution and said that you shouldn't stop your surveillance at five years because cyst size stability for five years doesn't preclude the future growth or development of cancer," he said. "There was nearly a three-fold increased risk of cancer compared to the general population."
In another paper, in which investigators followed patients after resection of IPMNs of the pancreas, the authors concluded long-term follow-up was necessary for detection of metachronous pancreatic cancer and malignant IPMNs after resection of IPMNs, Miller noted.
Various medical associations or societies have issued guidelines on the management of pancreatic cysts, with differences across guidelines.
"There are variations in the guidelines between different associations highlighting the lack of a uniform consensus," Miller said. "The majority of them all say if it's equal to or over 3 cm, then you have to worry about it."
The guidelines do not offer consistent information with respect to frequency and length of surveillance, Miller noted.
"What is important to recognize is that guidelines vary based on the target patient population, the type of clinical symptoms, the size of the cysts and the recommendations regarding the timing and duration of initial long-term imaging surveillance," Miller said.
Still another challenge with surveillance is the absence of markers to predict which patients with cysts will develop cancer in the cysts themselves or in the remainder of the pancreas, Miller pointed out.
And while it may sound enticing to use abbreviated MRI protocols with noncontrast MRI given the large number of small pancreatic cysts and associated potential for their lifelong follow-up, there is no evidence to support that abbreviated protocols with noncontrast MRI will not affect the rate of detection of pancreatic cancer, according to Miller.
"Until I have more evidence or guidance, I will continue to use contrast," he said, underlining the field defect complicates assessment.