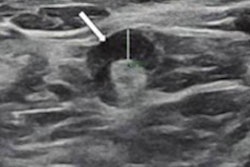
Researchers found that 1% of women vaccinated against COVID-19 who underwent screening mammography were recalled for ipsilateral adenopathy in a single-center study published January 26 in Academic Radiology.
A team led by Dr. Santo Maimone from the Mayo Clinic in Jacksonville, FL, found that it's possible to achieve low recall rates related to vaccine-induced adenopathy. These recalls can limit unnecessary workups, improve access, and allow for flexible timing of vaccinations and screening exams, the group wrote.
Ipsilateral adenopathy has been widely reported in patients as a reaction to the COVID-19 vaccines. For women with a history of breast cancer, swollen glands can be concerning. For breast radiologists, this means increased workloads that could lead to more unnecessary workup.
Researchers said the reported incidence of such adenopathy varies, with higher estimates in early reports and small series. Therefore, Maimone and colleagues wanted to find out callback rates linked to vaccine-induced adenopathy for women undergoing screening mammography.
They looked at data from 2,304 women. Out of these, 24 (1.0%) were recalled for ipsilateral adenopathy. The researchers found no significant difference in adenopathy presence linked to patient age, dose, or brand of vaccine.
They also found that the more days that passed since vaccination, adenopathy's presence significantly decreased (p < 0.001). Adenopathy was 10.5 times more likely and 0 to 14 days (p < 0.001) and 7.9 times more likely at 15 to 28 days (p = 0.002) than beyond 28 days. The receiver operating characteristic (ROC) curve also suggested that 28.5 days is the best cutoff point in determining how likely adenopathy will be present on a mammogram.
Among the 24 women called back, five were assessed as benign and 19 were assessed as probably benign. The latter were recommended for short-interval follow-up imaging for three months. The median time from initial recall to the decision to resume routine imaging was 98 days, with a range of 13 to 157 days.
However, nine patients have reportedly not returned for subsequent follow-up imaging, eight of whom were late for their initial three-month follow-up exam while the other one was ate for a second follow-up exam.
Despite this, the study authors reported that no cases resulted in biopsy or malignancy.
The team touted their results as being helpful in answering "many unanswered questions" about vaccine-induced adenopathy, including its workup and potential duration.
"It also provides an example of an achievable vaccine-induced adenopathy callback rate when patients' vaccine-related information is provided to the interpreting radiologist," they added.
For such results to be achievable, the researchers wrote that vaccine-related information must be accurate and given to radiologists at the time of the exam. They also called for radiologists to continue making recommendations based on individual imaging findings and clinical judgment, as well as future studies to validate their findings in other practices.