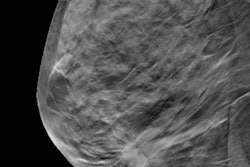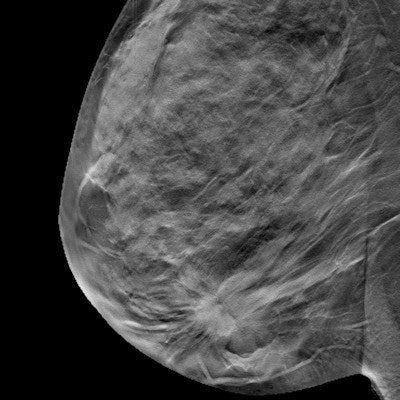
The evidence in support of digital breast tomosynthesis (DBT) just keeps rolling in. A recent study in Radiology found the technology sustained high specificity and low false-positive rates over multiple breast screening cycles.
 Dr. Manisha Bahl.
Dr. Manisha Bahl.Since its approval in 2011, DBT has grown in popularity as a screening method, thanks in part to its ability to simulate 3D visualization of breast tissue. The new study, which was published online on April 7, is the latest in a growing body of evidence finding the benefits of DBT may last through multiple screening rounds.
"We found that the benefits of reduced abnormal interpretation rate and improved specificity with digital breast tomosynthesis were sustained beyond the first DBT screening round," wrote the authors, led by Dr. Manisha Bahl of the department of radiology at Massachusetts General Hospital.
For their study, Bahl and colleagues reviewed tens of thousands of screening mammography results from women who visited an academic medical center for routine breast screening. The women who visited the center between March 2008 and February 2011 were exclusively screened with digital mammography, while those who visited between January 2013 and December 2017 received DBT.
| DBT vs. digital mammography for breast screening | ||
| Digital mammography | Digital breast tomosynthesis | |
| Cancer detection rate (per 1,000 examinations) | 4.6 | 5.3 |
| Abnormal image interpretation rate | 7.3% | 7.1% |
| Positive predictive value of recall | 6.3% | 7.4% |
| Sensitivity | 84.2% | 87.3% |
| Specificity | 93.1% | 93.4% |
DBT screening was associated with a higher cancer detection rate, lower abnormal image interpretation rate, and higher positive predictive value than digital mammography. It also had a higher sensitivity and specificity.
Furthermore, all but one year of DBT screenings had significantly lower odds of an abnormal imaging interpretation rate and significantly higher odds of specificity. Three of the DBT screening years (2, 3, and 5) also had a higher proportion of detected invasive cancers.
"Our study contributed to the existing literature by demonstrating that the reduction in [abnormal interpretation rate] was sustained after the first screening round," the authors wrote. "The decrease in unnecessary diagnostic imaging may result in savings in healthcare expenses, time, and resources; compensate for the additional time required to interpret DBT examinations; and reduce patients' anxiety."
The authors noted the findings often dropped out of statistical significance for year four of DBT examinations but not the prior years or year five. They attributed the phenomenon to a potential change in patient demographics or the experience level of reading radiologists.
The DBT and digital mammography cohorts also had a small but significant difference in age, race, breast density, and prior screening due to changes in the hospital's patient demographics. While the cohorts were different, the authors noted their findings still demonstrate the long-term value of DBT.
"Our results suggest that the benefits of digital breast tomosynthesis extend beyond the first screening round," the authors wrote. "In particular, the benefits of reduced false-positive examinations and higher specificity with DBT are sustained after the first screening round."