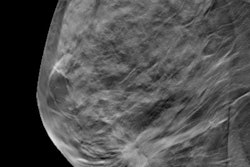
Most radiologists who are using digital breast tomosynthesis (DBT) for breast screening have synthesized 2D mammography capability, but they also have concerns about its image quality, according to a study published online August 12 in the Journal of the American College of Radiology.
The findings offer a snapshot of how synthesized 2D mammography is actually being used in clinical practice, wrote a team led by Dr. Samantha Zuckerman of the University of Pennsylvania in Philadelphia.
"Both single-center population-based studies and early reader studies have found similar or improved performance of synthesized digital mammography when used in place of digital mammography in DBT screening," the group wrote. "However, many breast imagers continue to have concerns about image quality, particularly as it relates to calcification characterization."
DBT has been rapidly implemented into clinical practice since the first system was approved by the U.S. Food and Drug Administration in 2013. Synthesized 2D is an enhancement to DBT that enables users to create a 2D image from DBT data, obviating the need to acquire a separate 2D image acquisition.
But it's unclear how breast imaging practices are using synthesized 2D mammography. Zuckerman's group sought to assess changing utilization patterns and attitudes among breast imagers regarding the technology.
To do this, the team sent an online survey in 2018 to Society of Breast Imaging members that included questions regarding practice type, use of DBT and synthesized 2D mammography, perception of change in recall and cancer detection rates with synthesized 2D mammography and DBT compared with digital mammography and DBT, and attitudes toward synthesized 2D mammography versus digital mammography in DBT screening. Of 2,600 members, 312 responded; the majority of respondents were in private practice.
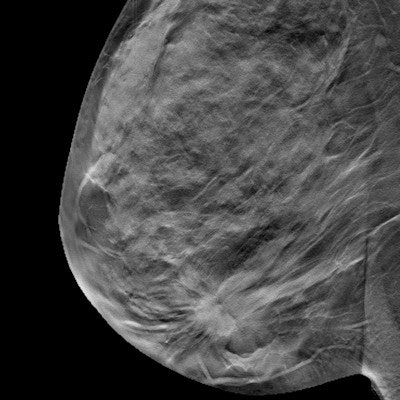
Most survey respondents (96%) reported having DBT in their practice, and 83% reported having synthesized 2D mammography capability. Of those who did not have synthesized 2D mammography, the most cited reasons were the cost of the software upgrade (32%) or image quality concerns (32%).
The researchers also found the following:
- Of the survey respondents, 52% reported synthesized 2D mammography use in the majority of DBT screens.
- 85% of survey respondents stated that the advantage of synthesized 2D mammography was decreased dose, while 27% cited increased lesion conspicuity.
- 61% stated that the disadvantage of synthesized 2D mammography was calcification characterization, while 31% cited decreased image quality.
- 31% of survey participants reported that using synthesized 2D mammography decreased recall rates, while 30% were unsure of the technology's effect on recall rate and 6% reported a recall rate increase.
- 21% reported an increase in the cancer detection rate using synthesized 2D mammography, while 44% were unsure of any cancer detection rate change and 1% reported a decrease.
On a scale of 1 to 5, overall satisfaction with synthesized 2D mammography was 3.4, the group noted.
The study findings show that DBT is now widely used by most breast imagers and in most breast cancer screening studies -- but concerns remain, according to Zuckerman's group.
"The majority of practices ... screening with DBT have synthesized digital mammography capability; however, [its] usage with digital mammography in DBT screening varies, as does radiologist satisfaction," the team concluded.