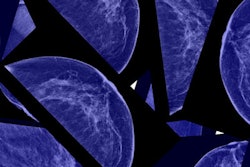
Does mammography really save lives? That's the question raised by a new study published July 17 in the Journal of the National Cancer Institute (JNCI), which analyzed data from Sweden to conclude that there is no evidence that mammography screening has an impact on mortality from breast cancer in the country.
The study is the latest research from a group led by Dr. Philippe Autier of the International Prevention Research Institute in Lyon, France. Autier's group has published several studies in recent years calling into question mammography's benefit, based on analyses of mortality data from large national screening programs.
But the group's research -- based on observational studies -- conflicts with randomized clinical trials that have demonstrated a mortality benefit for mammography. The conflict raises the question of which type of study is best-suited for analyzing mammography's benefits and harms, with some observers taking the position that the issue is so complex that it may be impossible to prove definitively.
Previous research
This week's paper is the third by Autier's group in the past 18 months on mammography. In a July 2011 paper in British Medical Journal, the group compared mortality rates at a number of European countries that implemented breast screening programs at different times. Because each nation had markedly different mortality reductions from breast cancer, the group concluded mammography screening did not play a major role in reducing deaths from breast disease.
The researchers reached a similar conclusion in a February 2011 paper in Annals of Clinical Oncology, where they compared mortality rates and incidence rates of advanced breast cancer across different countries with screening programs. While breast cancer mortality fell in all the countries they studied, Autier's group said the declines were already occurring before screening began, while incidence rates for advanced breast cancer didn't fall after a decade and a half of screening -- a sign that mammography was not catching cancer earlier.
In the new study, Autier and colleagues looked at mortality rates in different counties in Sweden that implemented mammography at different times, beginning in 1974, and compared them with expected mortality rates based on a statistical model they developed. The study noted that between 1972 and 2009, overall breast cancer mortality rates in Sweden have fallen, from 68.4 deaths per 100,000 women to 42.8 deaths per 100,000, an overall drop of 37% over 38 years.
If mammography were the reason for the decline, breast cancer death rates would begin falling first in the counties where screening was first implemented, and later at other counties. The researchers created five groups of counties based on when each one started their screening programs. The first group consisted of counties where breast screening began in 1974-1978, the second 1986-1987, the third 1987-1988, the fourth 1989-1990, and the fifth 1995-1997.
The researchers assumed that screening would begin to impact breast cancer death rates about six to 10 years after programs began, with the full impact occurring about eight years after that. Instead, the researchers found that breast cancer death rates varied widely by county groups: No change in trends occurred in the first two groups, while groups 3 and 4 saw mortality decline two to four years after screening began, but at a rate that indicated that screening mammography was responsible for a 5% to 8% reduction in mortality -- much lower than the mortality reduction of 23% and higher claimed in some of the randomized trials in Sweden.
"In the two groups of counties where screening started between 1974 and 1986, we found no evidence that mammography screening contributed to reductions in breast cancer mortality," the group wrote.
If not mammography, then what was behind the steady decline in breast cancer mortality in Sweden since 1972 -- a decline that was not seen in other European countries? Autier's group cited studies that have postulated that it would be due to better treatment, as "special attention was given to breast cancer patients in Sweden."
Observational versus randomized
Among the study limitations, Autier and colleagues noted that their study was observational in nature, as opposed to the randomized trials that are generally considered to be more scientifically rigorous. But the early randomized trials that reported a strong mortality benefit to screening suffered from flawed design, and, in any event, such trials may not be the best way to evaluate mammography, Autier stated in an email to AuntMinnie.com.
"Routine screening programs can be evaluated most readily by time trends and differential mortality from the disease for which screening is being performed," Autier wrote. "Case-control studies should not be used for evaluating the effectiveness of breast screening because they cannot disentangle the role of screening and of treatment in mortality changes."
Autier group's findings were discussed in a pair of editorials, one by Dr. Michael Vannier of the University of Chicago and the other by several authors led by Dr. Nereo Segnan of ASO S. Giovanni Battista University Hospital in Turin, Italy.
Segnan's group claimed that analyzing mammography's effectiveness by looking at time trends of mortality probably wasn't the most effective method. A number of factors can dilute the results of such studies, especially when trends are compared across different regions, as they are in the Autier research.
"The authors' conclusion that the important 'downward trends ... in breast cancer mortality in Sweden have evolved practically as if screening had never existed' seems to be difficult to justify and implausible," Segnan and colleagues wrote. "It is also partially unsupported by the data; two of the four groups of counties do show a mortality decrease that, according to the stated criteria, could be linked to screening."
For his part, Vannier wrote that the JNCI study highlights the challenges of using mortality statistics to calculate mammography's effectiveness.
One challenge is that screening events and mortality events are widely separated by time, he said in a conversation with AuntMinnie.com. Making a change in screening might not show an impact on mortality for a long period of time, and the Autier paper had a somewhat shorter follow-up period, he said.
Disease-specific mortality is also difficult to calculate due to the unreliability of death records, and many of the observational studies are problematic in that they track those who were invited to an intervention (mammography) but not necessarily those who completed it.
Adding to confusion
Ultimately, the Autier study will probably add to the confusion over mammography, especially when some findings such as those in the current study are used to make the argument that mammography screening shouldn't be offered, Vannier said.
"We have a lot of people looking at the same dataset and coming up with completely different conclusions," Vannier said. "It's disturbing, the conclusion from some that people shouldn't be screened at all. It makes sensational press, but it doesn't seem to really be helping anyone."
What the Autier research does accomplish is highlight the shortcomings of the current approach to mammography screening, in which high-risk women are lumped into the same category as low-risk women, based simply on their similar ages. The research community's understanding of the risk factors for breast disease is much more sophisticated than when mammography was first introduced in the 1970s, and our society's approach to screening should probably reflect that, Vannier believes.
"We can now calculate a woman's risk, and, in a sense, personalized medicine emerges," Vannier said. "You can separate those who need intensive screening ... from those who have much less risk. To have a one-size-fits-all approach doesn't really make sense."