Throughout this year's COVID-19 pandemic, chest CT has proved to be a valuable tool for diagnosing the illness in particular clinical situations -- such as when reverse transcription polymerase chain reaction (RT-PCR) testing isn't readily available or results are delayed.
But the modality has also shown value in assessing the severity of the disease and evaluating ongoing conditions that can plague recovered patients, especially when combined with artificial intelligence (AI), according to several presentations in a scientific session on chest imaging delivered Sunday at the RSNA 2020 meeting.
Predicting severity
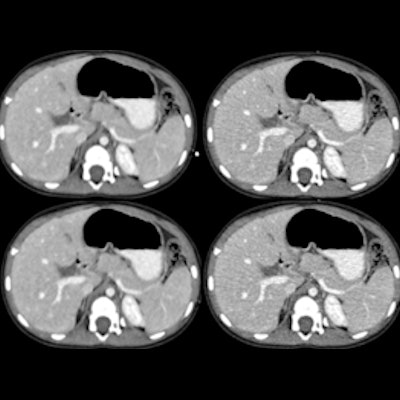
In the afternoon session, a team led by Ziyue Xu, PhD, senior scientist at graphics processing unit technology developer Nvidia, shared results from a study the company conducted that combined a deep-learning algorithm with chest CT to predict whether COVID-19 patients would be admitted to the intensive care unit (ICU).
The findings suggest that AI could boost CT's performance when it comes to helping clinicians predict COVID-19 severity, Xu told session attendees.
"[This deep-learning algorithm can] alert the clinician to the enhanced potential of ICU admission, when combined with other clinical features," he said.
For the study, Xu and colleagues included 632 chest CT scans from patients with COVID-19 confirmed by RT-PCR testing; of these, 69 patients were admitted to the ICU and 563 were not. The team developed a whole-lung segmentation algorithm and assessed its effectiveness when used with CT by overall accuracy, sensitivity, and specificity.
The algorithm achieved high accuracy, specificity, and negative predictive value (NPV) for identifying COVID-19 and predicting ICU admission on chest CT.
| Deep-learning algorithm's performance with chest CT for identifying COVID-19 and predicting ICU admission | |
| Measure | Performance |
| Accuracy | 92% |
| Sensitivity | 73% |
| Specificity | 93.9% |
| PPV* for predicting ICU admission | 53% |
| NPV for predicting ICU admission | 97% |
"Based upon chest CT alone, AI-based deep-learning algorithms can reasonably predict clinical outcomes such as ICU admission in patients with COVID-19 who underwent CT and PCR on the day of admission," Xu concluded. "The model is feasible with reasonable accuracy and specificity of prediction."
Predicting prevalence
In a second Sunday afternoon presentation, Italian researchers looked at whether CT's performance varied depending on the prevalence of COVID-19 disease in a region.
A group led by Dr. Marcello Petrini of Guglielmo da Saliceto Hospital in Piacenza, Italy, assessed the modality's diagnostic performance for severe illness by comparing an outbreak phase to an ensuing period of lower disease incidence (first outbreak, high prevalence: February 21 to March 7; second period, lower prevalence after 28 days of lockdown: April 6-13).
The researchers used RT-PCR results as the reference standard to evaluate CT's sensitivity, specificity, positive predictive value, and negative predictive value.
The high-prevalence group included 198 patients and the low-prevalence group included 146 patients. The team found that while CT had about the same sensitivity regardless of disease prevalence, specificity was lower during the time of higher disease prevalence:
| Chest CT's performance for diagnosing COVID-19 depending on disease prevalence | ||
| Measure | High-prevalence period | Low-prevalence period |
| Positive RT-PCR rate | 89% | 31% |
| CT sensitivity | 94% | 93% |
| CT specificity | 63% | 73% |
| CT PPV | 95% | 61% |
| CT NPV | 58% | 96% |
The study's main finding of a high PPV rate on chest CT during the early-outbreak, high-prevalence period in Italy and a high NPV rate during the second, low-disease-prevalence period should help clinicians more effectively manage patients suspected of COVID-19, Petrini concluded.
"Even with a negative CT, the likelihood to have COVID-19 pneumonia is still high during the high-prevalence phase of the disease while it is very low in the low-prevalence period," he said.
Identifying airspace
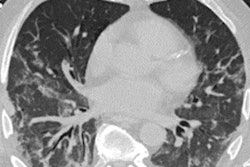
In the third Sunday afternoon talk, a team led by Dr. Eduardo Jose Mortani Barbosa of the University of Pennsylvania in Philadelphia noted that COVID-19 patients may develop airspace disease, in which alveolar air is replaced by fluid, pus, or blood and the condition continues beyond four to six weeks after treatment.
Chest x-ray is the go-to for evaluating this condition, but it tends to have limited sensitivity. While chest CT is more accurate, it's not used routinely to assess airspace disease.
Barbosa and colleagues developed a way to quantify the percentage of lung volume involved in airspace disease on chest x-rays using a convolutional neural network (CNN) algorithm based on 1,000 chest CT scans of COVID-19 patients. The researchers used a test set of 86 patients with positive RT-PCR results who had chest CT and chest x-ray less than 48 hours apart.
The algorithm projected the CT exams' 3D lung and airspace disease segmentation on reconstructed x-rays using quantitative maps of lung tissue thickness and manifestations of airspace disease.
The group found that the CNN-reconstructed x-rays quantified airspace disease at least as well as the human CT exam readers: CT had a rate of 24.3%, while the CNN's digitally reconstructed x-rays had a rate of 24.4%.
"This approach may increase efficiency and consistency in chest x-ray interpretation of COVID-19 patients, especially when applied to longitudinal chest x-ray data to inform management," Barbosa concluded.