A high rate of discrepancies on primary body MRI exams acquired at outside institutions such as community hospitals shows a clear need for second exam interpretations by subspecialists when patients are transferred to a new center, according to a study published online October 14 in the American Journal of Roentgenology.
Most of these errors are interpretive, noted the team led by Dr. Danielle Kostrubiak from the University of Vermont in Burlington.
"Secondary interpretations of body MRI at tertiary care centers identify a high rate of discrepancies -- with primary errors being interpretive in origin -- suggesting that subspecialty interpretations should be encouraged, and institutions should provide adequate resources for these interpretations to occur," the American Roentgen Ray Society (ARRS) said in a statement it released about the study.
Radiologists at tertiary care centers are often asked for secondary reads of imaging exams, especially for patients transferred from community hospitals, the investigators noted. Discrepancy rates between these readings can vary widely, but abdominal, pelvic, and cross-sectional studies tend to have the highest rates.
Although it is understood that there are often inconsistencies between prior imaging reports and secondary reads, the types of errors of which these inconsistencies consist have not been clear, according to the authors.
"We are not aware of any studies that have specifically focused on secondary interpretations of body MRI analyzed by type of likely error, and to our knowledge, ours is the largest MRI sample size published to date," the team wrote.
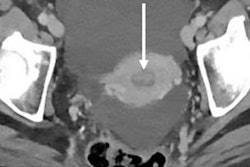
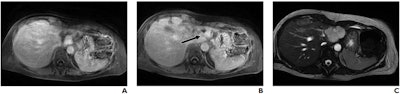 A 56-year-old woman with benign hemangioma. Lesion was originally reported as indeterminate enhancing mass, and outside report recommended biopsy. Classic features of benign hemangioma are shown. Error was attributed to faulty reasoning. (A) Axial MR image obtained five minutes after contrast agent administration shows peripheral nodular discontinuous enhancement. (B) Axial MR image obtained 10 minutes after contrast agent administration shows centripetal progression of enhancement (arrow). (C) Axial fast imaging employing steady-state acquisition (FIESTA) MR image shows lesion is homogeneously hyperintense compared with liver parenchyma. Images and caption courtesy of the ARRS.
A 56-year-old woman with benign hemangioma. Lesion was originally reported as indeterminate enhancing mass, and outside report recommended biopsy. Classic features of benign hemangioma are shown. Error was attributed to faulty reasoning. (A) Axial MR image obtained five minutes after contrast agent administration shows peripheral nodular discontinuous enhancement. (B) Axial MR image obtained 10 minutes after contrast agent administration shows centripetal progression of enhancement (arrow). (C) Axial fast imaging employing steady-state acquisition (FIESTA) MR image shows lesion is homogeneously hyperintense compared with liver parenchyma. Images and caption courtesy of the ARRS.Kostrubiak and colleagues identified 357 secondary MRI reports for body exams that were originally performed and interpreted at an outside center between January 2015 and December 2018. They compared the original report from the outside facility to the secondary interpretation conducted at the University of Vermont and categorized the cases as "discrepancy" or "no discrepancy." The group then further divided the exams by type of error: perceptive or cognitive.
The investigators found that 68.9% of the cases had at least one inconsistency between the original report and the secondary interpretation. Most reading errors were those of "faulty reasoning" -- that is, cognitive errors in identifying an abnormality -- at 34.3% of the total number of discrepancies identified between the reports and 37.8% of primary discrepancies.
The second most common error type was a perception error called "satisfaction of search," which the researchers found in 15% of overall discrepancies between the two reports and 37% of primary discrepancies. This type of error happens when the exam reader stops searching for abnormalities after identifying an initial one.
As more practices implement effective electronic medical record systems, evaluating report soundness should get easier, Kostrubiak and colleagues noted. But in any case, reducing discrepancies between primary and secondary imaging exam readings is crucial to improving patient care and reducing unnecessary healthcare costs, they wrote.
"The next step would be to explore how these discrepancies may impact patient outcomes and overall cost to the system associated with these radiologic errors," the group concluded.