Combining an MRI brain scan with blood test results could become a potent duo in producing clinically relevant information for glioblastoma patients and subsequently direct the most appropriate care for their disease, according to a study published February 27 in Neuro-Oncology Advances.
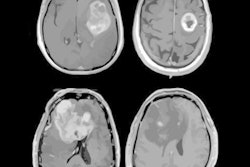
Researchers from the University of Pennsylvania (Penn) used MRI to image the blood-brain barrier and determine whether it could prevent cancer-related DNA (cfDNA) and tumor DNA (ctDNA) in the blood from entering the brain, which would fuel a recurrence or progression of glioblastoma.
"These findings represent an important step in understanding the factors that determine plasma cfDNA concentration and ctDNA detection, and hence the potential clinical utility of plasma-based liquid biopsy, in patients with glioblastoma," wrote the authors, led by Dr. Seyed Ali Nabavizadeh, an assistant professor of radiology at Penn.
Glioblastoma is a particularly aggressive form of cancer, with a five-year survival rate of only 5% to 10%. Even after treatment, the disease returns for almost all patients and does so in a mutated form, which requires repeat brain surgery.
One way to monitor glioblastoma is through blood samples, also known as liquid biopsies. These diagnostic tests measure both the amount of DNA (cfDNA) that cancer releases into the blood and the total amount of tumor DNA (ctDNA) in the blood.
Normally, the blood-brain barrier protects the brain from any infiltration of diseased blood, but cancer-related DNA can still slip through the blood-brain barrier and into the brain to exacerbate the glioblastoma. In this situation, MRI can play a pivotal role by determining how "leaky" the blood-brain barrier is. A porous blood-brain barrier would allow higher levels of cfDNA and ctDNA to enter a patient's brain.
For this study, the researchers analyzed tumor samples and results from 3-tesla MRI brain scans (Magnetom TrioTim, Magnetom Skyra, Magnetom Vida, Siemens Healthineers) of 42 adult patients (median age, 65 years; range, 20-81 years) with newly diagnosed glioblastoma. The protocol included dynamic contrast-enhanced (DCE) perfusion to assess blood-brain barrier integrity and help calculate amounts of tumor DNA circulating in the blood. Blood samples were collected immediately prior to surgery.
The study also found a correlation between the amount of cfDNA and the density of macrophages that account for a large percentage of the cells inside glioblastoma and represent a major barrier to the immune system fighting the tumor.
The researchers discovered a correlation between the amount of cfDNA and the density of macrophages inside the glioblastoma, which suggests that the "shedding of cfDNA into the blood is dependent on a sufficient level of blood-brain barrier disruption," the authors wrote. In addition, the increased tumor macrophage density and tumor size were associated with greater cfDNA concentration in the blood.
"This study is the first step toward a better understanding of the factors that influence plasma cfDNA concentration and somatic mutation detection in glioblastoma," Nabavizadeh and colleagues concluded. "Future studies are warranted to investigate the clinical utility of these findings to predict which subset of patients may benefit from liquid biopsy."