An artificial intelligence (AI) algorithm can predict how osteoarthritis (OA) will progress over four years based on analysis of baseline knee x-rays and other risk factors, according to research published online February 6 in Osteoarthritis and Cartilage.
After developing a model that blended assessment of traditional OA risk factors with deep-learning analysis of x-rays, a team of researchers led by Bochen Guan of the University of Wisconsin-Madison reported a high level of accuracy for predicting OA progression.
"The fully automated [deep-learning] models could be widely applied in clinical practice and clinical drug trials to rapidly predict the progression of radiographic joint space loss using readily obtainable demographic and radiographic risk factors and baseline knee x-rays," the authors wrote.
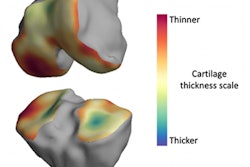
Developing OA risk-assessment models would be valuable for clinical practice and clinical drug trials, as current models based primarily on clinical and radiographic risk factors have only been moderately successful for predicting the incidence and progression of OA. Semi-quantitative and quantitative measures of knee joint pathology on baseline x-rays and MRI can improve risk assessment, but these imaging parameters are challenging to cost-effectively obtain, the team noted.
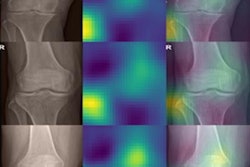
Hypothesizing that deep learning could yield a better method, the researchers created three different algorithms using a training set of 1,400 knees from the Osteoarthritis Initiative. The first -- an artificial neural network -- was developed to predict progression based on traditional demographic and radiographic risk factors. Next, the authors trained a deep-learning assessment model utilizing two convolutional neural networks (CNNs); the first CNN cropped the images and the second served as the classifier.
The third model combined the two previous algorithms, incorporating demographic and radiographic risk factors along with the deep-learning analysis of the baseline x‑rays as separate inputs. All models were then tested on a hold-out dataset of 400 knees. Progression of radiographic joint space loss was defined as a 0.7 mm or greater decrease in medial joint space between the baseline knee x-ray and the 48‑month follow-up x-ray.
| Performance for predicting progression radiographic joint space loss at 48 months | |||
| Traditional model (demographic and radiographic features) | Deep-learning model | Combined model | |
| Sensitivity | 61.5% | 78% | 80.5% |
| Specificity | 64% | 75.5% | 80.5% |
| Area under the curve | 0.660 | 0.799 | 0.863 |
The deep-learning model's increase in AUC over the traditional model was statistically significant (p < 0.001), while the combined model had a significantly higher AUC than both the traditional model (p < 0.001) and the deep-learning model (p = 0.015).
"The diagnostic performance of the combined joint training model compares favorably to other risk assessment models for knee OA reported in the literature, which have had AUCs ranging between 0.70 to 0.82 for predicting OA incidence," Guan and colleagues wrote.
The risk-assessment models now need to be further validated on different subject populations, according to the researchers.
"Future work is also needed to develop more comprehensive risk assessment models incorporating [deep-learning] analysis of baseline MR images for predicting the incidence and progression of knee OA," the authors concluded.