Prostate cancer imaging with PET/CT or PET/MRI and a gallium-68 (Ga-68)-labeled prostate-specific membrane antigen (PSMA) radiopharmaceutical works well, according to a study published in the August issue of the American Journal of Roentgenology.
Ga-68 PSMA with either PET/CT or PET/MRI modality achieved a sensitivity of 89% and a positive predictive value (PPV) of approximately 91% in a group of 150 patients who already had undergone a variety of treatments and surgery for their disease. The researchers found no serious adverse events in follow-up imaging.
The findings reinforce previous studies on Ga-68 PSMA's efficacy, according to the authors (AJR, August 2019, Vol. 213:2, pp. 266-274).
"Taken together with those of prior studies, our prospective results confirm high sensitivity and accuracy of PSMA-PET in this population and suggest an important role for this modality in guiding prostate cancer management in the future," wrote the researchers, led by Dr. Courtney Lawhn-Heath from the department of radiology and biomedical imaging at the University of California, San Francisco (UCSF).
Clinicians are increasingly relying on Ga-68 PSMA with PET/CT and PET/MRI to stage and restage intermediate- to high-risk primary prostate cancer and to guide and monitor response to therapies. An April 2019 study from researchers at The Wesley Hospital in Brisbane, Queensland, Australia, determined that five years after adopting the procedure, clinicians opted for Ga-68 PSMA PET/CT for the primary and secondary staging of prostate cancer in 95% of their cases.
While other large prospective trials have evaluated the efficacy of Ga-68 PSMA PET on patient care, "no prospective U.S. trials have evaluated the diagnostic accuracy and safety" of the modality, the authors noted. Therefore, the UCSF team set out to evaluate those two factors in this prospective study.
A total of 150 patients (mean age, 68.5 years; range, 47-86 years) underwent PET/CT (Discovery VCT, GE Healthcare) or time-of-flight PET/MRI (Signa, GE) approximately one hour after injection of Ga-68. The median dose was 199.8 MBq (± 48.1 MBq; range, 107.3-273.8 MBq).
The PET/CT protocol involved five-minute acquisition times per bed position from the pelvis through the midabdomen and three-minute acquisitions from the upper abdomen to the vertex. Whole-body PET/MRI scans were performed simultaneously and targeted the pelvis and abdomen with bed positions of eight minutes, and above the diaphragm with bed positions of three minutes. Ga-68 PSMA PET/CT and PET/MRI data were anonymized and interpreted by two blinded board-certified nuclear medicine physicians in random order.
"The primary endpoint was sensitivity on a per-patient and per-region basis. The pathologic result when available was considered the reference standard," the researchers explained. "In the absence of pathologic correlation for a lesion, validation of findings at Ga-68 PSMA-11 PET was evaluated on the basis of clinical and imaging follow-up."
Regarding the safety of Ga-68 PSMA-11 PET, 146 patients (97%) reported no adverse effects from the scans. The four remaining patients reported dizziness after imaging, a fall after the scan that was attributed to the furosemide injection, mild nausea for 24 hours, and mild constipation that appeared to be unrelated to the injection, respectively.
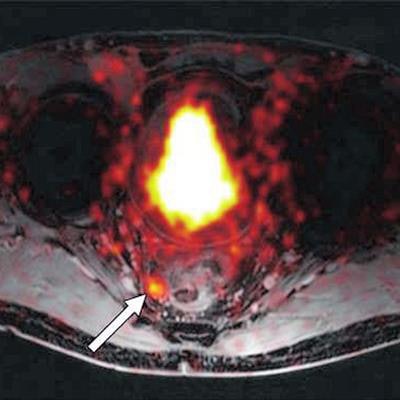
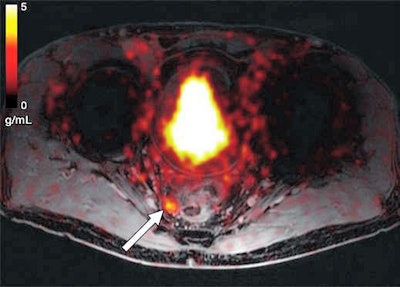 Axial Ga-68 PSMA-fused PET/MR image shows abnormal radiotracer uptake (arrow) within rounded right mesorectal lymph node. Transrectal biopsy findings were negative for malignancy. Patient underwent androgen deprivation therapy. Image courtesy of AJR.
Axial Ga-68 PSMA-fused PET/MR image shows abnormal radiotracer uptake (arrow) within rounded right mesorectal lymph node. Transrectal biopsy findings were negative for malignancy. Patient underwent androgen deprivation therapy. Image courtesy of AJR.On a per-patient basis, the mean sensitivity reached 89%, and the PPV was 90%. On the other hand, specificity was rather low at 31%, and the negative predictive value was 25%.
The researchers attributed the latter results to "the relative paucity of pathologic, imaging, and clinical follow-up," and "because specificity is related to both false-positive and true-negative findings, even a small number of false-positive findings drastically affected our measured specificity."