PHILADELPHIA - Providing lutetium-177 (Lu-177) prostate-specific membrane antigen (PSMA) radioligand therapy (PRLT) earlier to patients with metastatic prostate cancer can extend lives, according to research presented on Tuesday at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) conference.
While this therapy had previously only been used in patients with end-stage disease, German researchers found that patients who received Lu-177 PRLT earlier lived much longer than those who had received other treatments. What's more, 18 patients who received PRLT as a first-line therapy were still alive 55 months after treatment.
"These findings will help to determine the right place of [Lu-177] PSMA radioligand therapy in the treatment of metastatic prostate cancer -- for example, before chemotherapy -- and serve as a starting point for a prospective randomized controlled clinical trial," said lead author Dr. Harshad Kulkarni of the Theranostics Center for Molecular Radiotherapy and Molecular Imaging at Zentralklinik Bad Berka in Germany.
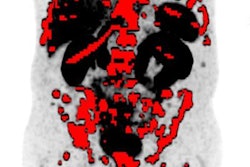
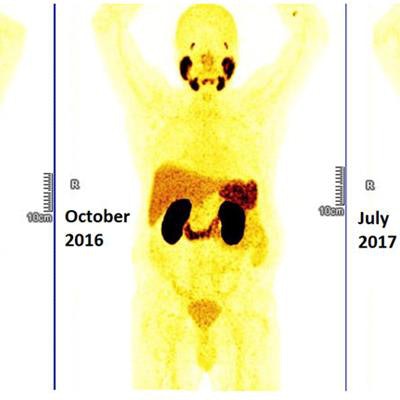
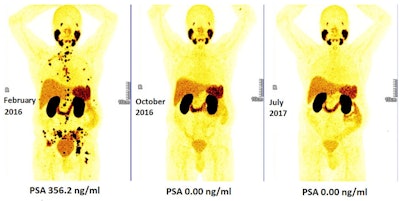 Persistent complete remission on long-term follow-up after early Lu-177 PSMA radioligand therapy. Lymph node and osseous metastatic, castration-resistant, and chemotherapy-naive prostate cancer in a 62-year-old patient demonstrated no evidence of disease on Ga-68 PSMA PET/CT eight months (center) and 17 months (right) after first PRLT treatment. Image courtesy of Dr. Harshad Kulkarni et al, Theranostics Center for Molecular Radiotherapy and Molecular Imaging at Zentralklinik Bad Berka in Germany.
Persistent complete remission on long-term follow-up after early Lu-177 PSMA radioligand therapy. Lymph node and osseous metastatic, castration-resistant, and chemotherapy-naive prostate cancer in a 62-year-old patient demonstrated no evidence of disease on Ga-68 PSMA PET/CT eight months (center) and 17 months (right) after first PRLT treatment. Image courtesy of Dr. Harshad Kulkarni et al, Theranostics Center for Molecular Radiotherapy and Molecular Imaging at Zentralklinik Bad Berka in Germany.The study included 224 patients with metastatic prostate cancer, who were restaged following diagnosis with gallium-68 (Ga-68) PSMA PET/CT as part of a theranostic nuclear medicine pairing, according to the researchers.
"This approach of precision oncology uses the concept of theranostics -- i.e., we see what we treat, and we treat what we see," Kulkarni said. "[Lu-177]-PRLT patients were selected and followed-up with [Ga-68] PSMA PET/CT, using the same ligand for molecular imaging and molecular radiotherapy."
The patients were grouped according to previous therapies they had received, including surgery, chemotherapy, and external-beam radiation therapy. The researchers monitored patients' prostate-specific antigen (PSA) levels before and after they received PRLT.
Of the patients who received Lu-177 PRLT, 157 (70%) had a reduction in their PSA level; 121 (54%) experienced a decline of more than 50%. First-line PRLT therapy was associated with the longest overall survival, as all 18 patients were still alive at 55 months, according to the researchers.
Those patients who were previously treated with chemotherapy had a significantly shorter survival rate: a median of 19 months. Survival was also shorter (median of 17 months) in patients who had received previous treatment with radium-223. Prior surgical or radiation treatment of the primary tumor did not significantly affect overall survival, however.
In other findings, the researchers reported that patients who had at least a 50% decline in PSA level after at least two PRLT cycles lived significantly longer -- a median of 38 months. What's more, additional treatment with the newer antiandrogen agents abiraterone or enzalutamide in combination with Lu-177 PRLT extended survival to a median of 40 months.
"Our study demonstrates a potential survival benefit and superior response after early initiation of [Lu-177] PSMA radioligand therapy," Kulkarni said. "PRLT was safe with no or minimal side effects. These results are, therefore, likely to have a significant impact on patients' lives -- maintaining their quality of life for longer."