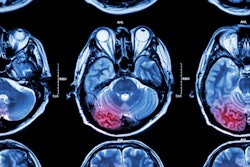
Determining which stroke patients should undergo mechanical clot removal hinges on a complex network of clinical imaging factors. Measuring collateral blood flow through CT angiography (CTA) can help optimize the process, according to a study published online September 25 in JAMA Neurology.
In a retrospective analysis, researchers from Massachusetts General Hospital identified poor blood flow in the collateral arteries as one of the chief variables that can lead to a deterioration of patient condition en route to thrombectomy, ultimately forcing clinicians to postpone the procedure.
Early detection of poor collateral blood flow using CTA could be vital for predicting infarct growth and subsequently improving triage efficiency, according to lead author Dr. Gregoire Boulouis, Dr. Arne Lauer, and colleagues.
"The ability to determine infarct evolution has the potential to allow optimized resource use within stroke networks by better selecting patients most likely to remain eligible and limiting futile transfers for thrombectomy," they wrote (JAMA Neurol, September 25, 2017).
Pressed for time
Evidence from six recent clinical trials demonstrated that thrombectomy, or mechanical clot removal, improves outcome in patients with acute ischemic stroke and large-vessel occlusion. These data triggered the American Heart Association to update its guideline, such that patients graded "6" or higher on the Alberta Stroke Program Early CT Score (ASPECTS) were recommended to undergo endovascular treatment.
A major hurdle with certain endovascular treatments, including thrombectomy, is that they need to take place in specialized centers located far away from the referring hospital. For example, stroke patients who are assigned to immediate thrombectomy arrive at these advanced stroke centers on average 3.2 hours later.
As patients travel from one site to the next, their infarction often worsens, occasionally so much so that they are no longer able to safely undergo the assigned surgical treatment. In a previous 2016 study, the research team found that 20% of patients transferred to their stroke center for endovascular therapy had to be excluded due to an enlargement of their infarction (JAMA Neurol, January 2016, Vol. 73:1, pp. 43-49).
Fortunately, a 2017 study by Mokin et al uncovered a key determinant of infarction progression -- the severity of a patient's stroke, as graded using the U.S. National Institutes of Health Stroke Scale (NIHSS). Patients with a clinical stroke severity of "6" or higher were deemed eligible to undergo thrombectomy, provided they were able to arrive within six hours of symptoms onset (Journal of NeuroInterventional Surgery, May 2017, Vol. 9:5, pp. 442-444).
Scoring patients, however, depends on a menagerie of clinical imaging factors, and not just stroke severity alone.
"In rapidly evolving stroke care networks, the question of the need for vascular imaging at the [referring hospitals] remains unsolved, resulting in an important amount of futile transfers for thrombectomy," Boulouis and colleagues wrote.
Clinical imaging factors
With this in mind, the researchers sought to hone in on the clinical and imaging factors that could help identify which patients are the best candidates for transfer. They retrospectively analyzed CT imaging for 316 patients transferred from 30 referring hospitals to a thrombectomy-capable stroke center between January 2010 and 2016.
Boulouis and Lauer reviewed the CT scans acquired from the referring hospitals and the CTA studies from the stroke center, focusing on the following variables: ASPECTS, presence and localization of dense vessels, presence and localization of vessel blockage, degree of collateral blood flow, and classification of infarction evolution based on the European Cooperative Acute Stroke Study criteria.
A decline in a patient's ASPECTS score (ASPECTS decay) was defined as a drop in patient score from above "6" at diagnosis to below "6" upon arrival at the stroke center, which would make patients ineligible for thrombectomy due to the increased size of the clot.
Analysis of the data revealed that stroke patients who experienced significant ASPECTS decay (p < 0.001) were most commonly characterized as follows:
- Female
- Not taking anticoagulants
- Having higher initial NIHSS
- Having a dense vessel sign on initial CT
- Having poor collateral blood flow on CTA
Taking the analysis one step further, the researchers created a model to determine how these factors affected the progression of infarction. This second model incorporated information from the CTA scans acquired after patients arrived at the stroke center.
"We assumed that if a proximal occlusion was found at the [stroke center], it would have been present if the CTA had been performed before transfer, and thus, we assigned the CTA proximal occlusion and collateral status to the patient while at the [referring hospital]," they explained.
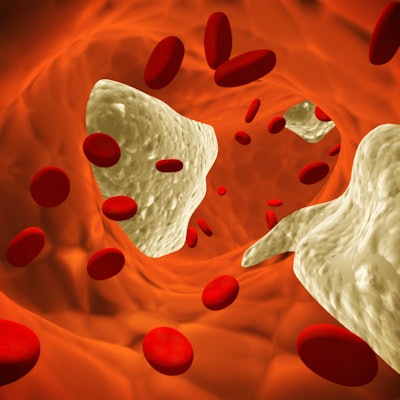
Collateral blood flow
This advanced model pointed to poor collateral blood flow as the most significant predictor of infarction progression toward ineligibility for thrombectomy, among the variables examined.
| Factors associated with infarction progression toward ineligibility for thrombectomy | ||
| Odds ratio | p-value | |
| Female | 1.55 | 0.32 |
| Initial NIHSS | 1.13 | < 0.001 |
| Initial ASPECTS | 0.33 | < 0.001 |
| Proximal arterial occlusion | 2.04 | 0.12 |
| Poor collateral blood flow | 5.14 | < 0.001 |
The researchers then expanded the study to include 330 patients with initially unfavorable imaging profiles. This dataset, too, highlighted poor collateral blood flow as a significant predictor of major infarction progression.
Pulling the results together, the researchers keyed in on the initial NIHSS score, the presence of a dense vessel or clot, and poor collateral blood flow as the main determinants of ASPECTS decay and, thus, unfavorable conditions for thrombectomy.
"Vascular imaging to identify intracranial occlusions and assess collateral blood vessels may provide an additional tool for determining triage decisions when transferring a patient," they wrote.
Effect on stroke assessment protocol
What impact should the results have on the use of imaging in assessing stroke patients?
Currently, the initial NIHSS scores and the presence of clots are both assessed with CT before patients are transferred, and collateral blood vessel status is typically determined via CTA after patients arrive at specialized stroke centers.
But it's critical to minimize delays in stroke patients with no or poor collateral blood flow. So it might be best to include CTA with the initial stroke assessment, recommended Dr. Bruce Campbell, PhD, from Royal Melbourne Hospital in Australia, in an accompanying editorial in JAMA Neurology.
"CT angiography should be performed immediately after the noncontrast CT of the brain at the first hospital that assesses the patient," Campbell wrote.
Acquiring CTA images of patients with ischemic stroke at the referring hospitals before they are selected to undergo thrombectomy is supported by these findings, Boulouis and colleagues concluded. And yet, they also recognized the difficulty of shifting clinical protocol.
"Implementing refinements of patient triage through vascular and collateral imaging at the [referring hospital] represents an organizational challenge," they wrote. "The added value of vascular imaging and collateral blood vessel assessment for decision-making regarding transfers requires further evaluation and adequate tailoring to local resources and needs."