We report the case of a pregnant patient who developed massive life-threatening hemobilia as a result of cholangiohepatitis with extensive hepatolithiasis involving both lobes of the liver. Selective hepatic angiography showed an arteriobiliary fistula arising from the right hepatic artery, which was successfully treated with arterial embolization. We review the published literature concerning Oriental cholangiohepatitis associated with hemobilia and draw conclusions for the management of similar cases in the future.
Case report
A 33-year-old woman pregnant for 12 weeks was admitted to an outside hospital with a history of Oriental cholangiohepatitis and clinical evidence of ascending cholangitis with severe hemobilia. An ultrasound performed on admission revealed extra- and intrahepatic bile duct dilatation and gallstones.
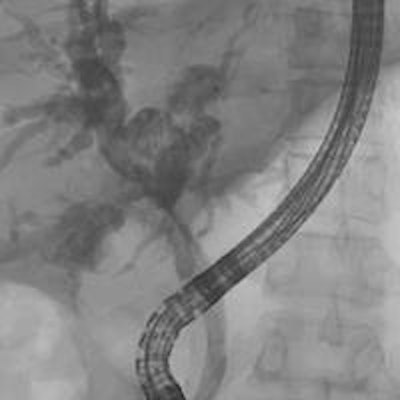
The patient first underwent an endoscopic retrograde cholangiopancreatogram (ERCP) with placement of two biliary stents. After initially improving for a few days, the patient developed hematemesis and the pain recurred. A second ERCP again showed extensive hepatolithiasis in both liver lobes obstructing both hepatic ducts, and active bleeding was observed from the common bile duct. Four units of packed red blood cells were transfused to the patient (figure 1).
However, the patient's clinical condition continued to deteriorate, and she was transferred to our hospital with hemoglobin of 57 g/L that necessitated transfusion of an additional four units of packed red blood cells. Despite aggressive resuscitation, the patient remained hemodynamically unstable with systolic blood pressure periodically dropping into the 80-90 mm Hg range. Hence she was brought as an emergency to interventional radiology for further management.
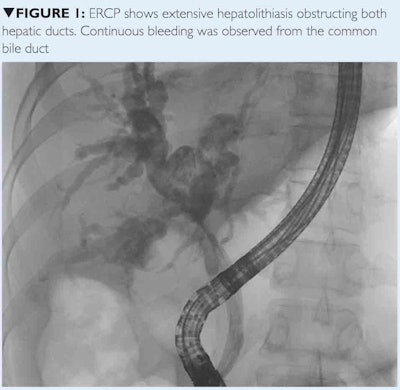
With appropriate shielding, a selective hepatic angiogram was performed that showed brisk active extravasation from the proximal right hepatic artery, just distal to the origin of the middle hepatic artery. The remaining arterial branches were unremarkable. Operative repair was deemed infeasible by the hepatobiliary surgeon. Therefore, transcatheter arterial embolization (TAE) was performed using Gelfoam and microcoils.
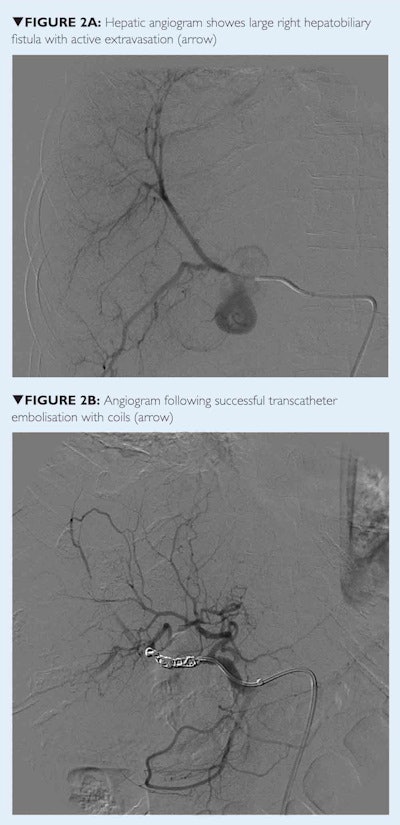
A postembolization angiogram showed complete occlusion of the right hepatic artery with no evidence of active extravasation remaining and the patient stabilized. The following week she underwent a cholecystectomy, extrahepatic bile duct excision, intrahepatic stone removal, and hepaticojejunostomy.
Discussion
Hemobilia is defined as bleeding into the bile ducts due to abnormal communication between a blood vessel and the bile duct. Severe or recurrent bleeding requires active intervention, and major hemobilia can present as a life-threatening hemorrhage, as it did in this case. With rapid bleeding, the blood flows directly into the duodenum and can manifest as hematemesis or melena. Slower bleeding results in blood clotting in the bile ducts, and the patient may present with obstructive symptoms.
Different etiologies have been implicated as causes of hemobilia, with trauma representing a large percentage of cases. This includes accidental trauma and iatrogenic injuries such as surgery, percutaneous transhepatic cholangiography, and liver biopsy. Other causes include liver abscess, radiofrequency ablation, ERCP, and liver transplantation in children.
Early recognition and management of arteriobiliary fistula is extremely important to prevent life-threatening complications. Endoscopy is required to rule out other causes of upper or lower gastrointestinal hemorrhage. Many patients will undergo CT scanning, especially in cases of trauma or suspected arterial injury. This can show cavitating lesions, aneurysms, or pseudoaneurysms.
While initial management is conservative, major hemobilia will usually require definitive treatment. Traditional surgical options include liver suturing, partial hepatic resection, or hepatic artery ligation depending on the location of the lesion. With advances in endovascular therapies, transcatheter arterial embolization has become a viable option.
The choice between surgery and TAE depends on the cause and site of bleeding, the type of pathology, and the general condition of patient. As surgery can have high rates of morbidity and mortality, TAE is considered the treatment of choice in high-risk patients.
The goal of transcatheter embolization is to decrease pulsatile flow distal to the occlusion rather than devascularizing the hepatic parenchyma. Different temporary or permanent embolizing materials may be used, including Gelfoam compresses, steel coils, or polyvinyl alcohol (PVA) particles.
The complication rate after TAE is low due to the dual blood supply to the liver from the portal vein and hepatic artery. Known complications include hepatic necrosis, abscess formation, nontarget embolization, gallbladder infarction, and, rarely, catheter-induced artery damage. Other complications are related to angiographic technique and include access site hematoma, dissection, or pseudoaneurysm. The patient may have transient elevation of liver enzymes and may develop self-limited postembolization syndrome.
Conclusion
Transcatheter embolization is safe, reliable, minimally invasive, and effective in the management of life-threatening hemobilia. It is preferred in high-risk patients due to a significant reduction in morbidity and mortality compared with surgery.
Note: Since this case report was written, the patient has delivered.
Dr. Huda Ahmed Al Braiki is a radiology resident at Sheikh Khalifa Medical City (SKMC) in Abu Dhabi, United Arab Emirates. Dr. Asim Ahmed Khwaja is chair of the radiology department at SKMC and a consultant in interventional radiology.
Acknowledgment
Dr. Muhammad Zaman, kidney transplant and hepatobiliary surgeon, SKMC.
References
References available upon request ([email protected])
Copyright © Arab Health magazine, Issue 1, 2014



















