VIENNA - Every general radiologist can sometimes be involved in a potentially embarrassing situation when a colleague demands help in solving a problem about the nipple and areolar area of a patient whom he or she is concerned about. What results can be expected from an ultrasound? Is it indicated or not? A presentation at Thursday's breast ultrasound course aims to answer those questions and provide an update on developments within breast ultrasound.
In an interview with ECR Today, Dr. Rafael Salvador, an associate professor of radiology and director of breast imaging at the Breast Unit at University Hospital Vall d'Hebrón in Barcelona, Spain, admits it is difficult to find out much about the nipple and areolar region in any textbook or scientific literature.
"But this part of the breast adds specific skin and dermal pathology to the more known ductal or stromal breast pathology," he said. "Furthermore, the relation of benign versus malignant pathology differs a lot from the rest of the breast."
Ultrasound is the more simple and accessible technique to image this area. It's important to remember benign lesions are much more frequent than any other (infiltrating, noninfiltrating, or even premalignant), and thus ultrasound becomes useful for diagnosis as well as to control the evolution. Another reason ultrasound is the method of choice is that it's cheaper than MRI.
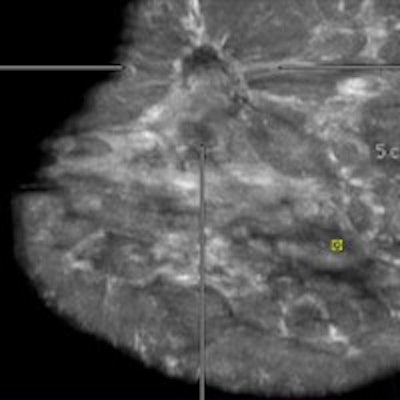
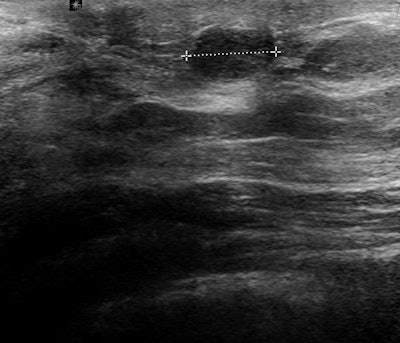 Ultrasound of the subareolar region shows a superficial 8-mm, round, solid, homogeneous tumor that turned out to be a papilloma. This is the most frequently found benign tumour in this part of the breast. Image courtesy of Dr. Rafael Salvador.
Ultrasound of the subareolar region shows a superficial 8-mm, round, solid, homogeneous tumor that turned out to be a papilloma. This is the most frequently found benign tumour in this part of the breast. Image courtesy of Dr. Rafael Salvador."The main advantage of ultrasound for nipple/areolar region is the chance to do a physical examination combined with the results of the technique in a single session," he continued. "The special tricks and facts to consider about the technique and a thorough knowledge of the pathology of nipple and areola will help the radiologist in achieving a high performance in the approach to a clear diagnosis in this part of the breast."
It is very important that radiologists are not afraid to check the nipple and areola under ultrasound in patients with problems in this area. It is necessary to convince the clinicians that ultrasound will add many facts to refine the diagnosis and treatment for their patients, he noted.
In terms of the future, the increasing number of interventional procedures, mainly percutaneous excision of papillomas and other benign subareolar lesions, reflects a trend to use ultrasound intervention to reduce open surgery for these superficial lesions.
Update on automated breast ultrasound
In the hospital as well as in private practice, general radiologists in many parts of Europe are dealing with the entire array of imaging modalities in their routine work, according to Dr. Michael Fuchsjäger, head of the department of general radiology at Medical University of Graz in Austria. Breast imaging is an integral part of general radiologists' work, and many of them are working in mammography screening programs. During his presentation, ECR delegates will get firsthand information on a new development in breast ultrasound, which will be mainly used to complement screening mammography: automated breast ultrasound.
 Dr. Michael Fuchsjäger from the Medical University of Graz in Austria.
Dr. Michael Fuchsjäger from the Medical University of Graz in Austria.This technology is based on computer generation of a 3D imaging dataset obtained from many parallel 2D images. It offers a different approach with a variety of benefits, he said. Images are obtained by the sonographer in a standardized fashion; whole breast datasets can be reviewed at any time after the examination, which reduces operator dependence, and image fusion with MRI, for instance, is possible.
Automated breast ultrasound is indicated in screening patients in whom incidental cancers would be expected, according to Fuchsjäger. Scientific studies show automated breast ultrasound's highest value is for high-risk screening populations -- i.e., patients younger than 50, with dense breast tissue, a personal history of breast cancer, or a genetic risk.
"Automated breast ultrasound would fit perfectly as a complement to screening mammography in women with heterogeneous dense or very dense breast tissue (BI-RADS composition 3 or 4)," he stated. "It is not intended to replace handheld breast ultrasound, which is the method of choice for evaluation for suspicious lesions, preoperative staging, axillary lymph nodes assessment, as well as ultrasound-guided breast interventions."
While automated breast ultrasound won't replace handheld ultrasound, there are some significant differences. Some of handheld ultrasound's strengths are that it's widely available, relatively inexpensive, and well tolerated by women. Also, any interventions can be readily performed; respective biopsy equipment is cheaper than for other imaging modalities.
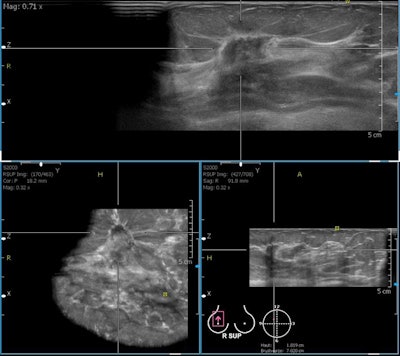 A 76-year-old woman with invasive ductal cancer of the right breast. Automated breast ultrasound shows extremely hypodense, irregular, spiculated mass lesion with dorsal shadowing (BI-RADS 5). Notice coronal view on the bottom left with retraction feature of invasive cancer not seen in transversal or sagittal views. Image courtesy of Dr. Maria Bernathova, Medical University of Vienna.
A 76-year-old woman with invasive ductal cancer of the right breast. Automated breast ultrasound shows extremely hypodense, irregular, spiculated mass lesion with dorsal shadowing (BI-RADS 5). Notice coronal view on the bottom left with retraction feature of invasive cancer not seen in transversal or sagittal views. Image courtesy of Dr. Maria Bernathova, Medical University of Vienna."With handheld ultrasound you are close to your patients -- that is so important in breast imaging, where clinical examination and clinical history are highly relevant for imaging diagnoses," Fuchsjäger explained. "After the area of the 'invisible radiologist' (see Radiology, January 2011, Vol. 2581: pp. 18-22), it is important to understand that radiology is a 'clinical' specialty in medicine. Breast ultrasound, whether handheld or automated, brings us closer to our patients, helping us in making a correct diagnosis consistently."
However, handheld ultrasound is a highly operator- and experience-dependent modality. Real-time adjustments (gain, focal zones, dynamic range, pressure, etc.) are necessary for good results, and abnormalities have to be recognized at examination, otherwise they are missed. With automated breast ultrasound, on the other hand, there are standardized views (like in mammography) for better reproducibility. Acquisition is separated from interpretation, and second reading, like with screening mammography, is an option, he continued.
"It saves a physician time, as examinations can be performed by technologists," he said. "Furthermore, first trials report a higher cancer detection rate for automated breast ultrasound and mammography versus mammography alone."
Limitations include lower ultrasound frequency than for handheld devices, no Doppler analysis or elastography imaging, difficulty in scanning the axillary region, and the relatively large amount of data (0.7-1.0 GB per examination). Artifacts can be an issue due to the bigger transducer (15 cm).
When asked what ECR delegates will get out of his lecture, Fuchsjäger wrote: "Attendees will understand the physics of handheld and whole-breast ultrasound, they will become familiar with the practical technique of handheld and whole-breast ultrasound, and they will be able to appreciate the clinical applications of handheld and whole-breast ultrasound, including automated screening."
Originally published in ECR Today on 6 March 2014.
Copyright © 2014 European Society of Radiology



















