The combination of 3D imaging technology with PET/CT holds the potential for diagnostic lesion characterization and preprocedural planning for a host of clinical indications, according to a pilot study conducted at Stanford University's molecular imaging program and the departments of radiology and bioengineering in Stanford, CA.
"This technique appears to show potential for guiding surgical procedures and for adding important diagnostic information that may herald new applications for the use of PET/CT," wrote the study authors in this month's Journal of Nuclear Medicine (July 2006, Vol. 47:7, pp. 1081-1087).
The scientists tested a new 3D imaging and processing protocol on 24 patients (11 male and 13 female, with a median age of 64) with various malignancies to determine whether it could dependably acquire and reformat standard 2D PET/CT images into 3D renderings. There were eight cases of lung cancer, two cases of lymphoma, five colorectal cancer cases, four esophageal cancer cases, two cases of breast cancer, and one case each of pancreatic cancer, cervical cancer, and head/neck cancer among the patient cohort.
Out of the study group, 21 patients were referred by oncologists for staging or restaging with FDG-PET/CT and contrast-enhanced CT. Three of the patients had an FDG-PET/CT virtual colonoscopy, two of whom were referred because an abnormal lesion was found during conventional colonoscopy, and one recruited without prior knowledge of colonic abnormalities, according to the researchers.
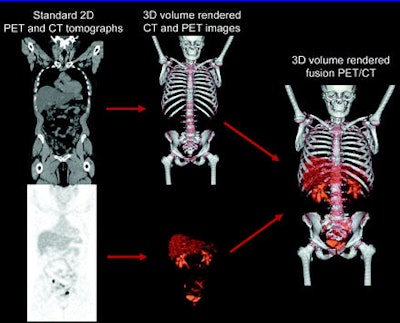 |
| Standard 2D tomographic CT and PET images, which contain scaling and alignment parameters calculated by software on the PET/CT scanner, are simultaneously rendered into a single image that combines CT anatomy and PET activity in correct anatomic relationship. Bone, soft-tissue, and airway windows can be selected when using 3D rendering of CT to emphasize a particular anatomic perspective. A similar process is used to create 3D-rendered virtual endoscopy images. Image and caption courtesy of and copyright © 2006 by the Society of Nuclear Medicine. |
The patients were imaged on either a Discovery LS or a Discovery ST (GE Healthcare Chalfont St. Giles, U.K.) PET/CT system and received 370-666 MBq of F-18 FDG after a minimum 12-hour fast. An unenhanced whole-body CT was performed for attenuation correction after tracer uptake (45-75 minutes), which was then followed by a whole-body PET scan in 2D mode at four minutes per bed position, with six or seven bed positions. In 21 of the 24 patients, a contrast-enhanced chest CT was also performed.
"The detector configuration of the Discovery LS scanner was not capable of imaging with optimal overlap for 3D reformatting and therefore was suboptimal by current 3D CT reformatting standards; this suboptimal protocol was used on four of the 24 patients," the authors noted.
The three patients who underwent FDG-PET/CT virtual colonoscopy had a modified protocol of the department's standard CT colonography procedure. They fasted and underwent a bowel-cleansing regimen similar to other CT colonoscopy studies and had 518-592 MBq of F-18 FDG administered intravenously, allowing approximately 45 minutes for tracer uptake. The patients were in control of air insufflation of their bowel during the exam, and were asked to periodically reinsufflate at 30- to 45-second intervals during the study.
"The entire scanning sequence consisted of prone CT, prone PET, a two- to three-min rest, supine CT, supine PET, and supine PET without air insufflation," the group wrote. "Air insufflation is particularly difficult with PET because the scanning time is several-fold longer than with CT."
The authors noted that, on the basis of their initial experience with the technique, that prone PET/CT acquisition with air insufflation provided better image quality and that they may omit supine acquisitions in future protocols to minimize patient discomfort and shorten imaging time.
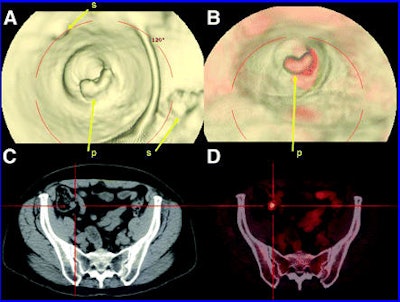 |
| CT virtual colonoscopy compared with PET/CT virtual colonoscopy for detection of a potentially malignant lesion. (A) CT-based virtual colonoscopy showing several areas of stool that are difficult to distinguish from potential malignant polyp. (B) PET/CT virtual colonoscopy showing intense F-18 FDG uptake that highlights suspected polyp relative to surrounding stool and greatly aids in differentiation of lesion from stool. (C and D) Retrospective review of standard 2D PET/CT tomographic slices reveals abnormal focus in colon that was missed on original interpretation (C) and would not have been detected without 3D fusion rendering (D). p = polyp; s = stool. Image and caption courtesy of and copyright © 2006 by the Society of Nuclear Medicine. |
The scientists used GE's proprietary Volume Viewer Plus software to create five image sets for each patient for physician review. The image sets included a standard 2D PET, 2D CT, 2D PET/CT, 3D-rendered external-perspective PET/CT, and 3D-rendered internal-perspective PET/CT.
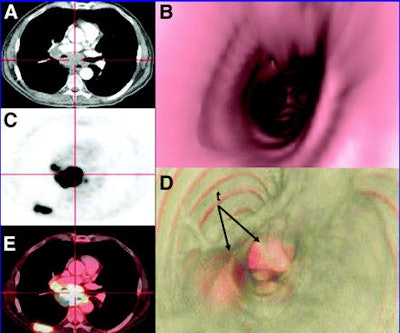 |
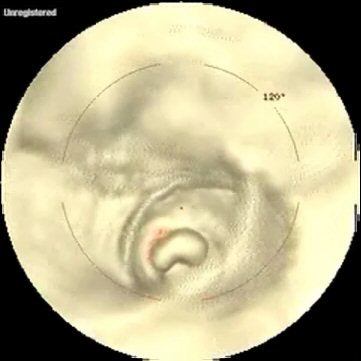
| CT virtual bronchoscopy compared with PET/CT virtual bronchoscopy. (A, C, and E) Standard 2D PET/CT tomographs show a patient with highly F-18 FDG-avid malignant subcarinal/paratracheal mass that extends along right tracheal sidewall and right bronchus. (B) CT virtual bronchoscopy illustrating that tracheal sidewall and carina appear normal, without indication of large tumors that abut central airways. (D) PET/CT virtual bronchoscopy showing abnormal F-18 FDG uptake along right paratracheal wall, carina, and proximal right bronchus consistent with regions of malignant tissue that were not evident on CT virtual bronchoscopy. Images and video fly-through provided excellent preview of region before surgical bronchoscopy. t = tumor. Image and caption courtesy of and copyright © 2006 by the Society of Nuclear Medicine. |
In an e-mail to AuntMinnie.com, lead author Dr. Andrew Quon noted that generating the PET/CT 3D datasets required some patience.
"The datasets varied considerably in time depending on the size and complexity of the tumor," he wrote. "Some of the tumors that encased structures were particularly challenging because it would take time for the 3D tech to 'carve out' the best view and select the proper opacity so that both the CT and PET images could be seen in 3D at the same time without one modality obscuring the other. I would estimate that these took approximately 15-60 minutes. Also realize that this was the first time we were working with these images and the software package for the fly-throughs (internal perspective) was completely proprietary and new, that is, the software was being tweaked as we went along."
The resulting image sets were then reviewed by a board-certified radiologist experienced in 3D imaging and a nuclear medicine physician experienced in PET/CT. The standard 2D image sets were reviewed first, followed by a review of the 3D PET/CT image sets.
Dr. Quon told AuntMinnie.com that the 3D dataset interpretation did not add all that much time to the diagnostic read by the radiologist and nuclear medicine physician.
"Interpreting the images did not take nearly as long as processing," he wrote. "The 3D images served an adjunctive role to the standard transaxial, coronal, and sagittal slices. The standard stacks of images still take significantly longer to interpret than the 3D rendered fly-around and fly-throughs. We really studied the 3D images intensely only in those special cases where there was a specific question or problem that wasn't answered on the standard slices -- although as mentioned in the study article, one case really surprised us on 3D in the colon. I would say less than five to 10 minutes for the 3D image interpretation component if I were reading the images purely clinically and not counting the fact that we poured over all the images because we knew it was a part of this experimental protocol."
In addition to the image interpretation, a surgeon or interventional radiologist reviewed the 2D PET/CT and 3D PET/CT images both before and after performing procedures, such as biopsy or endoscopy, and assessed the usefulness of the datasets in their decision on the type of procedure that was performed.
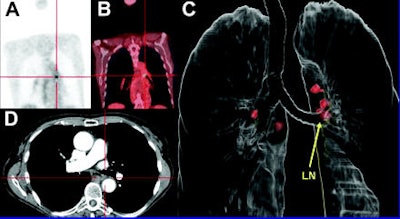 |
| 3D-rendered PET/CT fly-around aiding spatial localization of metastatic lymph nodes. (A, B, and D) Standard 2D tomographic F-18 FDG PET/CT images illustrating abnormal focus in left side of mediastinum, posterior to left bronchus (demarcated by red crosshairs). Despite coregistration of focus to contrast-enhanced thin-slice CT, it was difficult to detect and spatially localize lesion. (C) External 3D-rendered PET/CT fly-around showing abnormal F-18 FDG PET focus hidden behind left mainstem bronchus, as well as several additional perihilar F-18 FDG-avid lymph nodes. This image allowed clear spatial localization of lesion and guided mediastinoscopy biopsy. LN = lymph node. Image and caption courtesy of and copyright © 2006 by the Society of Nuclear Medicine. |
The diagnostic image interpretation team found that all 42 of the foci that were originally detected on the 2D PET/CT images could also be detected on the 3D PET/CT datasets. They also found that that the new technique appeared to aid in two of the 24 cases, allowing for the detection of a possible second primary lesion in a patient who presented for lymphoma restaging and underwent a PET/CT colonoscopy, and a switch from chemoradiation to surgical resection in a patient who presented for esophageal restaging.
 |
 |
| In this patient, the lesion was overlooked on the original interpretation of the standard 2D PET/CT images and would not have been adequately evaluated by CT-based virtual colonoscopy alone because of the large amounts of fecal matter. Video and caption courtesy of and copyright © 2006 by the Society of Nuclear Medicine. |
In the patient who underwent the PET/CT colonoscopy, the researchers noted that the CT portion of the exam was suboptimal because of the presence of a large amount of stool, attributed to inadequate bowel cleansing. They found that the 3D PET/CT scan was able to differentiate a polyp from fecal matter because of its intense (standardized uptake value of 7.8) FDG uptake.
The esophageal restaging patient's 3D PET/CT external-perspective image demonstrated a direct extension of an elongated distal esophageal tumor past the gastroesophageal junction and into the stomach.
The interventional radiologists and surgeons who participated in the study believed that 3D PET/CT aided in highlighting the location of lesions in all cases (six) that required a subsequent endoscopic exam, the researchers reported.
 |
 |
| Based partly on the 3D images, the surgeon selected mediastinoscopy over bronchoscopy (which was the original choice determined from 2D imaging). The 3D images also directed the route of the mediastinoscopy. Video and caption courtesy of and copyright © 2006 by the Society of Nuclear Medicine. |
Although the study was a proof of concept rather than a validation of technique, the scientists were heartened by the results and are working on creating further studies to include tracers other than FDG and anatomic regions other than the chest and colon. Dr. Quon believes that rubidium- or ammonium-based cardiac PET/CT studies are potential candidates for the application 3D technology.
"Clinically, 3D PET/CT fusion will most likely first be used most often in cardiac applications," he wrote. "I think it's the best and most obvious indication and there already are several groups working on this. Certainly our group intends to apply this technology to FDG and ammonia in the near future, and we are particularly interested in applying the idea to novel molecular imaging probes beyond Rb82 and NH3."
By Jonathan S. Batchelor
AuntMinnie.com staff writer
July 27, 2006
Note: Additional video files from the study are available for viewing at the Society of Nuclear Medicine Web site.
Related Reading
Part I: Medical image processing has room to grow, July 4, 2006
Imaging's big future gets smaller, July 3, 2006
Image-guidance system goes beyond bronchoscopy to access lung masses, June 14, 2006
Cardiac SPECT/CT fusion captures SNM's Image of the Year, June 6, 2006
3D rendering captures SNM's Image of the Year, June 21, 2005
Copyright © 2006 AuntMinnie.com