In a blow to mammography advocates, the U.S. Preventive Services Task Force (USPSTF) today changed its recommendation on mammography screening to advise women to start at age 50 rather than at 40.
In an article published November 17 in the Annals of Internal Medicine, USPSTF researchers announced that the agency was raising to 50 the recommended age at which breast screening should start. The USPSTF since February 2002 had recommended screening mammography, with or without clinical breast examination (CBE), every one to two years for women ages 40 and older.
"The USPSTF recommends against routine screening mammography in women aged 40 to 49 years," the recommendation now states. "The decision to start regular, biennial screening mammography before the age of 50 years should be an individual one and take into account patient context, including the patient's values regarding specific benefits and harms."
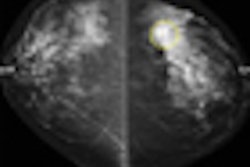
In announcing the change, USPSTF researchers said they had examined the efficacy of five breast screening modalities in reducing breast cancer mortality: film mammography, clinical breast examination, breast self-examination, digital mammography, and breast MRI. The agency conducted a systematic evidence review of six questions related to the harms and benefits of screening, and also performed a decision analysis that used population modeling to compare the expected health outcomes and resource requirements of starting and ending mammography at different ages, and using annual and biennial screening intervals.
In making the change, the USPSTF acknowledged that "there is convincing evidence that screening with film mammography reduces breast cancer mortality," but that the evidence is stronger for women ages 50 to 74 than for women ages 40 to 49. The strongest evidence is for the 60 to 69 age group. The agency found no evidence of a benefit to screening for women older than 75, and also no evidence to support clinical breast examination beyond mammography.
What's more, the agency also found the evidence "lacking" to support the use of digital mammography and breast MRI as a substitute for film mammography.
The USPSTF also made note of the harms involved in early detection and intervention, such as unnecessary imaging tests and biopsies in women without cancer, and inconvenience due to false-positive screening results. Also worth noting are the treatment of cancers that would not become apparent in a woman's lifetime, as well as the treatment of cancers that would become clinically apparent but would not shorten a woman's life. Radiation from mammography was noted as a minor concern, according to USPSTF.
The USPSTF has toughened its recommendation as to the frequency of screening as well. In 2002, the task force suggested women older than 40 undergo screening mammography every one to two years.
Now, in addition to shifting the screening age from 40 to 50, the USPSTF clearly recommended biennial screening, stating that "the evidence reviewed by USPSTF indicates that a large proportion of the benefit of screening mammography is maintained by biennial screening, and changing from annual to biennial screening is likely to reduce the harms of mammography screening by half."
In an editorial that accompanied the task force's new recommendations, Dr. Karla Kerlikowske at San Francisco Veterans Affairs Medical Center wrote that biennial screening of women ages 50 to 69 years averts 70% to 90% of breast cancer deaths attainable with mammography screening.
"About two additional breast cancer deaths are averted per 1,000 women who receive screening annually," Kerlikowske said. "Annual screening increases costs, which includes doubling the number of mammography examinations, false-positive results, and breast biopsies, and increases the chance of overdiagnosis."
Adding fuel to the fire
The USPSTF's announcement adds fuel to an ongoing controversy in the public policy world over mammography, as recent headlines have questioned whether mammography is truly effective at younger ages.
For example, an editorial on October 21 in the New England Journal of Medicine questioned the effectiveness of both mammography and prostate screening. With respect to breast cancer screening, the editorial noted that the incidence of cancer has risen following the introduction of mammography screening and has never returned to prescreening levels. This was taken to mean that screening is finding many cancers that may not pose a risk to patients, according to the authors.
The editorial prompted the American Cancer Society (ACS) to waffle in its support for mammography, first stating in a New York Times article that the agency might reexamine its own guidelines on mammography screening (which currently advise that it start at age 40), and then issuing a statement reaffirming its support for mammography screening.
Other groups have been quick to denounce the new USPSTF recommendations. The American College of Radiology (ACR) of Reston, VA, said that the new advisory was "unfounded" and the recommendations "ignore the valid scientific data" and will place women at risk, according to Dr. Carol Lee, chair of the ACR's Breast Imaging Commission.
"These unfounded USPSTF recommendations ignore the valid scientific data and place a great many women at risk of dying unnecessarily from a disease that we have made significant headway against over the past 20 years," Lee said. "Mammography is not a perfect test, but it has unquestionably been shown to save lives -- including in women ages 40 to 49. These new recommendations seem to reflect a conscious decision to ration care."
Another group, the Seattle Cancer Care Alliance, also had unkind words for the USPSTF's switch, as voiced by Dr. Constance Lehman, medical director of radiology and director of breast imaging at the Seattle Cancer Care Alliance. She is also professor and vice chair of radiology at the University of Washington School of Medicine.
"According to the ACS, 17% of breast cancer deaths in 2006 were among women who were diagnosed between ages 40 and 49," Lehman said. "We know that digital mammography significantly improves the detection of cancer in young women and in women with dense breast tissue. These well-documented facts are not included in the analyses that led to the change in recommendations."
By Brian Casey
AuntMinnie.com staff writer
November 16, 2009
Related Reading
JAMA editorial raises questions about breast, prostate screening, October 22, 2009
Shock and awe over JAMA editorial, October 22, 2009
'Spontaneous regression' debate erupts anew at ASCO symposium, October 12, 2009
Most breast cancer deaths seen in nonscreened women, October 7, 2009
Study traces steady declines in U.S. cancer deaths, August 13, 2009
Copyright © 2009 AuntMinnie.com