Gallium 67 Infection and Inflammation Imaging:
Gallium Imaging Technique:
The typical dose of Gallium is 5-6 mCi for infection (image at 6, 24 or 48 hours). When performing a total body scan a slow scan speed (10 cm/min.) is recommended in order to obtain adequate count densities. Spot images should be obtained for 10 minutes or 750,000 counts using three Gallium peaks. At least a medium energy collimator is required. A high energy collimator (364 KeV rated) will further reduce undesirable scatter, but also reduce overall count rate and lengthen imaging time. When performing spots of the abdomen the liver should be shielded or placed out of the field of view. Dual isotope imaging with 99mTcSc imaging may be performed to subtract liver activity. When imaging axillary abnormalities the arms should be raised above the head to fully expose the axilla as overlap of the axillary folds may simulate adenopathy.
Infection/Inflammation:
Gallium-67 is a group IIIb transition metal similar to the ferric ion and binds to multiple iron binding moecules including transferrin, lactoferrin, and siderophores [7]. In general Gallium activity parallels acute inflammation, returning to normal as the disease process resolves. Accumulation of Gallium at sites of inflammation/infection is multifactorial and related to:
- Increased capillary permeability and increased extravascular fluid associated with increased blood flow.
- Viable PMN's: Incorporate 10% of 67Ga bound to lactoferrin in intracytoplasmic granules and transport it to the lesion(s).
- B-Lymphocytes: Have lactoferrin binding sites on their surface which have a high affinity for gallium.
- Macrophages: Engulf protein-iron complexes and cellular debris, thereby accumulating gallium.
- Direct bacterial accumulation: Bacteria and fungi have an iron transporting mechanism. Siderophores (low molecular weight proteins) on the cells' surfaces bind gallium and facilitate its transport into the cell as a gallium-siderophore complex. This is one reason why neutropenic patients may still accumulate gallium within an abscess.
- Accumulation is increased in proportion to increases of osteoblastic activity in bone.
|
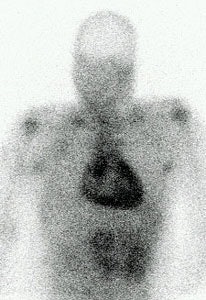
Myocarditis: This is a case of a patient with myocarditis. Note the intense cardiac gallium accumulation. Any inflammatory condition can result in increased gallium accumulation. CT scan demonstrated a small pericardial effusion. |
|
|
Osteomyelitis:
The role of Gallium in osteomyelitis imaging is discussed in the In-111 WBC Imaging section
Fever of Unknown Origin:
Fever of unknown origin is defined as a febrile illness evolving over 3 weeks, with a documented temperature of at least 38.3 degrees C (101 degrees F) on three or more occasions and uncertain diagnosis after one week of a diagnostic work-up in the hospital [6].
Either Gallium-67 or In-111 WBC imaging can be used for the evaluation of FUO. Gallium may be the agent of choice for initial screening of patients with FUO as approximately 20% of these patients have an occult neoplasm- especially lymphoma, leukemia, renal cell carcinoma, or hepatoma. Despite this fact, abscesses still account for 30-40% of the cases of FUO and although Ga67 imaging is perfectly acceptable for abscess detection, bowel activity and soft tissue activity can confound exam interpretation. In-111 WBC imaging is a reasonable alternative for the evaluation of patients with FUO [6]. Sensitivity has been reported to be between 55-85%, and specificity between 74-94% [6]. In a meta-analysis Ga67 had a pool sensitivity of 60%, a specificity of 63%, and a diagnostic yield of 35% (defined as the proportion of patients in whom the test results contributed to identifying the cause of the FUO) [8].
Pulmonary Disorders:
Pulmonary imaging is performed at least 48 hours following injection due to persistent nonspecific pulmonary activity which can be seen at 24 hours in about 50% of patients. Unfortunately, increased pulmonary uptake of Gallium is not diagnostic of any particular disease and can be seen in multiple disorders. Correlation with the clinical history is therefore essential. Bronchoalveolar lavage does not appear to increase Gallium uptake in subsequent images. Nonetheless, it is probably prudent to postpone lavage until after the completion of the Gallium exam. False-positive scans may result when the Gallium exam is performed within 2 to 3 weeks of open lung biopsy.
Adult Respiratory Distress Syndrome:
Acutely, pulmonary uptake is probably related to the increased capillary permeability associated with the disorder. Later uptake is probably related to the various cells involved in cellular proliferation and interstitial inflammation. Clinical improvement is associated with a corresponding decrease in Gallium uptake.
Asbestosis:
Increased pulmonary accumulation of Gallium is seen in the majority of patients with asbestosis and can occur prior to the appearance of radiographic abnormalities or functional impairment (40% of cases). Gallium accumulation has been shown by bronchoalveolar lavage to correspond to the early macrophage mediated peribronchiolar alveolitis that precedes the interstitial changes in the disorder. The degree of Gallium uptake has been shown to correspond to the degree of inflammation present. Gallium can therefore be used to identify an early asbestos-induced pulmonary process that may or may not lead to pulmonary fibrosis.
Drug Induced Pulmonary Toxicity/Hypersensitivity Pneumonitis:
Bleomycin, Nitrofurantoin, Cyclophosphamide, Methotrexate, and Amiodarone have all been associated with pulmonary toxicity. Gallium uptake can be seen prior to the appearance of radiographic abnormalities and is more sensitive to the detection of early toxicity. There is usually low to moderate increased uptake of Gallium.
Pneumocystis Pneumonia:
PCP generally presents with an acute onset of tachypnea and hypoxia. The CXR is normal in up to 40% of cases. The sensitivity of Gallium scanning for the evaluation of PCP in HIV patients has been reported to be as high as 90-95%. In PCP, there is generally diffuse increased pulmonary activity which is disproportionate to the clinical and radiographic findings. Unfortunately diffuse pulmonary Gallium accumulation can be seen in many other conditions which may affect these patients (CMV, MAI, M. tuberculosis, bacterial pneumonia, lymphoma, and cryptococcal infections) and therefore is non-specific (50-75%). Focal or patchy accumulation of the tracer can be seen in patients with PCP, particularly those who have been partially treated, but this pattern may also be seen in patients with superimposed bacterial infection. The specificity of the exam can be increased if one considers the intensity and distribution of the Gallium accumulation: Diffuse heterogeneous pulmonary activity which is more intense than the liver has a specificity for PCP between 95 and 100%. Diffuse homogeneous activity which is more intense than the liver has a slightly lower specificity for PCP of between 85 and 90%. If the intensity of the lung uptake is less than the liver, the specificity falls to 50% since this may reflect other types of diffuse underlying lung disease including viral infection (CMV), LIP (also look for parotid uptake), or post-drug treatment lung injury [4]. Nodal activity suggests granulomatous infection with TB or MAI. In patients who respond to treatment, pulmonary uptake of Gallium has been observed to return to normal.
Due to the presence of concurrent liver disease in these patients, determination of lung uptake relative to the liver may result in false-negative interpretations. A grading scheme of pulmonary uptake relative to the sternum should be more consistent.
- Grade 0: Normal
- Grade 1: Equivocal (Findings are probably not significant)
- Grade 2: Increased activity less intense than the sternum
- Grade 3: Increased and equal to the sternum
- Grade 4: Activity greater than the sternum
PCP is generally associated with at least grade 2 activity, and grade 3 and 4 are typically associated with significant disease.
|
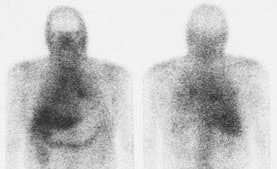
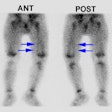
PCP pneumonia: This is a case of PCP pneumonia in an HIV patient with grade 4 tracer accumulation int he lungs (Note the associated colitis) |
|
|
Pulmonary capillary permeability using Tc-DTPA aerosol has also been evaluated as a means for diagnosing PCP infection. Increased permeability in patients with PCP results in a more rapid clearance of tracer from the lungs (see pulmonary imaging for further discussion).
Lymphocytic Interstitial Pneumonitis (LIP) can also be seen in HIV patients, particularly children. Parotid accumulation which is seen in LIP may aid in differentiating this disorder from PCP.
Sarcoid:
Sarcoid is a systemic disease process which involves the lungs in up to 90% of patients. Hilar nodes are involved in over 80% of cases. Peripheral lymph nodes, the liver, spleen, kidneys, eyes (iritis or iridocyclitis), CNS, heart, and skeleton may also be involved. Almost 50% of patients are asymptomatic and the great majority of patients have only a self-limited disease (65%). Pulmonary symptoms include dyspnea and a dry cough. Systemic signs include fatigue, weakness, and fever. Angiotensin converting enzyme levels are elevated in 30 to 80% of patients with active disease but are not specific for sarcoidosis. Although 20-30% of patients may be left with permanent pulmonary dysfunction the disease proves fatal in only about 5% of cases secondary to cor pulmonale. The disease likely begins as an alveolitis comprised of macrophages and lymphocytes (particularly T-lymphocytes) and progresses to granuloma formation and subsequently fibrosis. Sarcoid is staged by the plain film findings: Stage 0: Normal CXR; Stage 1: Hilar/Mediastinal nodal enlargement; Stage 2: Nodal and pulmonary parenchymal disease; Stage 3: Parenchymal disease only; and Stage 4: End stage pulmonary fibrosis.
Pulmonary accumulation of Gallium in patients with sarcoid is associated with active disease (either alveolitis or granulomas) and there is good correlation between the intensity of Gallium accumulation and the severity of disease as assessed by both biopsy and bronchoalveolar lavage. Gallium may also detect extrapulmonary sites of disease in the lacrimal, salivary, and parotid glands in up to 50% of patients. Inactive or fibrotic disease does not demonstrate increased Gallium accumulation. It is generally agreed that corticosteroid therapy is unlikely to benefit a patient with a negative 67Ga exam as this treatment is most effective during the inflammatory phase of the disorder. Unfortunately, a positive exam does not distinguish patients who will improve spontaneously (without treatment) from those who require medical intervention. Gallium scintigraphy has a sensitivity of 70% for detecting parenchymal disease, and a 95% sensitivity for hilar adenopathy. Overall sensitivity is about 90%. The thallium exam is usually negative in sarcoid.
|
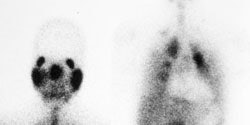
Sarcoid on Ga67 exam: The exam demonstrates diffuse pulmonary accumulation of the tracer consistent with active disease. Hilar acitivity appears asymmetric- but bilateral hilar activity can be seen (left more prominent on anterior image, right more prominent on the posterior image). SPECT imaging (not performed) would likely aid in assessment of mediastinal adenopathy. |
|
|
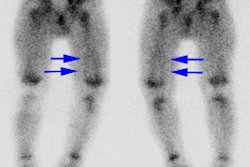
Mikulicz's syndrome (uveoparotid fever) is characterized by parotid, lacrimal, and bilateral salivary involvement. The disorder produces a characteristic gallium pattern referred to as the "Panda sign" (due to lacrimal, parotid, and physiologic nasophrayngeal Ga-67 activity). The Panda sign can also be seen in sarcoid patients without uveoparotid syndrome- in fact, it can be seen in up to 80% of patients with Stage I disease [3]. The panda sign can be seen in 4% of patients without sarcoid including lymphoma, Sjogren syndrome, and HIV [3].
|
Panda sign: Marked parotid and lacrimal uptake of gallium in this patient with sarcoid produces the classic "Panda" sign (left). In the chest, there is bilateral hilar and right paratracheal adenopathy, as well as active lung disease. |
|
|
PET scanning utilizing F-18 FDG has also demonstrated uptake within lymph nodes involved with sarcoid, extrathoracic lesions, and associated erythema nodosum [2].
Other disorders which can result in diffuse pulmonary accumulation of Gallium include:
- Lymphangitic carcinomatosis
- Pneumoconiosis: Silicosis
- Idiopathic Pulmonary Fibrosis (Usual Interstitial Pneumonitis): Degree of abnormal uptake is proportional to the activity of the inflammatory process. Uptake is often diffuse but heterogeneous due to the patchy nature of the disorder.
- Connective Tissue Disorders: Pulmonary uptake of Gallium is observed only occasionally.
- Following lymphangiogram
- Acute Radiation Pneumonitis
Gallium Imaging in AIDS:
Although Gallium is extremely useful in the evaluation of pulmonary pathology in HIV patients, febrile AIDS patients without localizing signs should be studied with In-111 WBC's (donor cells may be used as necessitated by the clinical setting) [1].
Up to 75% of HIV patients will demonstrate very prominent colonic accumulation of 67Ga, even in the absence of clinical symptoms. Gastric uptake is uncommonly seen (10%), but can be associated with lymphoma or infections such as: Candida (look for esophageal activity), Cryptosporidium (look for small bowel activity) or CMV (look for colonic and ocular activity. Hilar nodal activity is very uncommon).
REFERENCES:
(1) Radiology 1989; 170: 677-80
(2) J Nucl Med 1994; Lewis PJ, Salama A. Uptake of fluorodeoxyglucose in sarcoidosis. 35(10):1647-9
(3) Radiology 2000; Kurdziel KA. The panda sign. 215: 884-885
(4) J Nucl Med 1989; Ganz WI, Serafini AN. The diagnostic role of nulcear medicine in the acquired immunodeficiency syndrome. 30: 1935-1945
(5) Radiology 1989; Kramer EL, et al. Diagnostic implications of Ga-67 chest-scan patterns in human immunodeficiency virus-seropositive patients. 170: 671-76
(6) J Nucl Med 2002; Kjaer A, Lebech AM. Diagnostic value of 111In-granulocyte
scintigraphy
in patients with fever of unknown origin. 43: 140-144
(7) J Nucl Med 2016; Scherer PM and Chen DL. Imaging pulmonary inflammation. 57: 1764-1770
(8) AJR 2023; Palestro CJ, et al. FDG PET in evaluation of patients with fever of unknown origin: AJR expert panel narrative review. 221: 151-162