New research presented at this month's Genitourinary Cancers Symposium in Orlando, FL, indicates that imaging could be both overused and underused for prostate cancer patients, generating millions in unnecessary costs while also depriving some high-risk men of the benefits of imaging.
Lead author Sandip Prasad, MD, a fellow in oncologic urology at the University of Chicago Medical Center, said the overuse of imaging scans such as MRI, CT, and PET in low-risk and intermediate-risk patients could possibly account for a yearly unnecessary expenditure of $35 million in the Medicare population alone.
However, at the same time, imaging could be underutilized in patients with high-risk disease, with only 61% of subjects in Prasad's study receiving imaging to help stage disease. That number should be 100%, he believes.
"The 61% [figure] in patients who need imaging studies to properly stage them for treatment is very concerning," he told AuntMinnie.com. The overuse in low-risk and intermediate-risk patients wastes money; the underuse in high-risk patients could cost a man his life, Prasad said.
In low-risk and intermediate-risk patients, guidelines suggest there is no need for imaging scans that look for metastases because the chance of actually identifying a metastatic lesion in these individuals is small. "Studies have shown that the chance of finding a lesion with the scan is less than 1%," he said.
"We think that the percentage of low-risk patients getting these exams should be 0%," he said, citing guidelines from the American Urological Association and the National Comprehensive Cancer Network.
Similarly, Prasad said 0% of men diagnosed with intermediate-risk prostate cancer should be getting these scans -- yet his study, based on data from the Surveillance, Epidemiology, and End Results (SEER-Medicare) government database, showed that 49% of men diagnosed with this type of prostate cancer underwent imaging for staging.
While those tests may be wasting scarce resources, Prasad said he was more concerned that 39% of men diagnosed with high-risk prostate cancer -- and for whom guidelines recommend additional tests -- did not receive any imaging studies.
"All of these men should have received the tests," Prasad said.
In his study, 9,640 men were newly diagnosed with low-risk prostate cancer, 12,966 with intermediate-risk prostate cancer, and 7,577 with high-risk prostate cancer.
To put the cost of the unnecessary tests into perspective, Prasad noted that "$35 million is more than 10% of the annual budget of the National Cancer Institute for prostate cancer research."
Defensive medicine?
As is so often the case in imaging overuse stories, defensive medicine is believed to be the culprit.
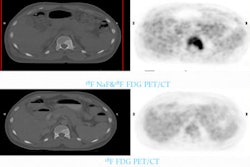
"I think there may be an aspect of defensive medicine as the reason for some of these tests, as well as an attempt by doctors to make sure they haven't missed anything when prescribing definitive treatment," Prasad suggested. The most frequently ordered tests were PET scans.
Prasad and colleagues found that overuse was observed most often in men who were older, black, and wealthier, and who resided in rural areas, while adherence to guidelines was found most often among men with higher education.
"Despite existing guidelines, costly and unnecessary imaging studies continue to be performed in men with low-risk and intermediate-risk prostate cancer, while a significant number of men with high-risk disease do not receive adequate staging prior to treatment," he said.
The results made Oliver Sartor, MD, director of the Tulane Cancer Center at Tulane University School of Medicine, shake his head.
"I know what doctors are thinking when they order these tests in low-risk individuals," Sartor said. "They just want to make sure their patient doesn't have that very small chance of having a metastasis. But just about every time, these tests just waste money."
Sartor said he could not fathom why high-risk prostate cancer patients with Gleason scores of 8 or higher, prostate-specific antigen (PSA) greater than 20, and a digital rectal examination that finds a lesion outside the gland would not have been sent for an imaging study.
"I'm not surprised to see these figures," commented Badar Mian, MD, an associate professor of surgery in the division of urology at Albany Medical College. "And I do find these figures concerning."
Overuse of scans is more likely to occur in private practices than at academic institutions, according to Mian. "At academic institutions, residents such as Dr. Prasad perform critical checks and balances by being encouraged to question various procedures," he said. "In other situations, doctors may just be going by gut feelings on the need for these tests."
The unnecessary tests may have cost the American taxpayer $35 million -- even considering the low rate of reimbursement under Medicare formulas, Prasad said.
"When you consider that private insurers for younger men may reimburse at a higher rate, the unnecessary expense may be far higher," he explained.
The symposium was cosponsored by the American Society of Clinical Oncology (ASCO), the American Society for Radiation Oncology (ASTRO), and the Society of Urologic Oncology (SUO).