Routine presurgical functional MRI (fMRI) provides "superior assessment" of the spatial relationship between brain tumors and the motor cortex, which, in turn, enhances the risk-benefit evaluation for patients before surgery, according to a study published online February 10 in European Radiology.
With that additional information, researchers at University of Heidelberg Medical School concluded, fMRI can positively alter patient treatment and reduce postoperative morbidity and hospitalization time. The lead author of the study was Martina Wengenroth, MD, from the university's department of neuroradiology.
In the study, Wengenroth and colleagues noted that while MRI provides excellent soft-tissue contrast and lacks ionizing radiation, the modality's results are "often compromised by large interindividual anatomical variability, even in healthy subjects."
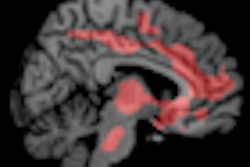
On the other hand, fMRI can provide diagnostic information noninvasively before surgery by assessing brain activity through the detection of local blood-flow changes that reflect neuronal activity of functional areas.
Patient population
The study included 77 consecutive patients: 42 female and 35 male subjects, with a mean age 51 years, ranging from 16 to 80 years. All 77 patients had brain tumors in the central region and received conventional 1.5-tesla MRI and fMRI before potential neurosurgical operation.
Tumors were localized in the left hemisphere in 38 patients and in the right hemisphere in 37 patients. Two patients had multiple metastases affecting both hemispheres. Due to the lesions, 29 patients experienced motor deficits, 21 had somatosensory deficits, and 10 had both motor and somatosensory deficits at the time of MR imaging.
With the conventional MRI scans, all patients received an intravenous injection of a gadolinium-based contrast agent (Magnevist, Bayer HealthCare Pharmaceuticals, or Omniscan, GE Healthcare) at a standard dosage of 0.2 mL/kg. All fMRI exams were performed with standardized blood-oxygen level-dependent (BOLD) technique with T2-weighted imaging.
Motor skills
During the scans, patients were asked to perform a series of motor skills tests, which included up and down movements of the tongue with closed lips, complex finger tapping with sequential finger-to-thumb movements, and repeated toe flexing and extensions without moving the ankles.
In the parts of the brain hemisphere with no tumors, conventional MR images showed that the thickness sign (the precentral gyrus and its cortex layer) and the hand knob (the motor hand area in the precentral gyrus) were the most reliable anatomical landmarks in 76 (99%) and 75 patients (97%), respectively.
In the tumor-affected hemisphere, however, the same landmarks could only be identified in 38 (49%) and 66 (86%) patients, respectively. In 11 cases (14%), conventional MR images were unable to identify the motor hand area at all based on the anatomical criteria.
By comparison, localization of the motor hand area with fMRI was still possible in all but one case, according to the researchers. "Thus, additional functional MRI was significantly superior to morphological MRI regarding the motor hand area localization," Wengenroth and colleagues wrote. "Motor areas of the foot and tongue were investigated in 70 patients and could be robustly identified in 97% (68/70) and 96% (67/70) of patients, respectively."
Because reliable morphological landmarks are not available for motor foot and tongue areas, these representations could only be located employing the fMRI technique.
Treatment management
Based on tumor origin and fMRI data, the decision was made for neurosurgery in 52 (68%) of the 77 patients. Among the 49 patients for whom complete resection was recommended, three received only partial resection.
The remaining 25 patients, who were initially scheduled for surgery, did not undergo any operation and received more conservative treatment, such as radiation and/or chemotherapy. For nine of the 25 patients, the decision for this course of action was based more on their poor clinical condition or the characteristics of the brain lesion.
In the other 16 patients, the decision to bypass surgery was based on the fMRI results, which portended major neurological impairments if surgery were performed. "Without exception, these 16 tumors were of malignant origin, mainly gliomas of different stages," the researchers wrote.
As for the patient outcomes, the study found that the clinical status for 12 patients improved after neurosurgery, 15 patients showed mild or temporary impairment, and four patients presented with severe postoperative neurological impairment. There was no change in neurological functions in 19 patients.
"In other words," the authors concluded, "fMRI-based risk assessment before surgery had a high correlation with the clinical outcome achieved and corresponded in 88% (46 out of 52 postoperative patients) with only minimal deficits or even functional improvement."