
By Shepard Hurwitz, MD and Philip E. Lucas, MB, BS, DRACR
Republished with permission from Applied Radiology, August 2000
Chronic foot and ankle pain is a common clinical problem in which it is often difficult to locate the anatomic source of pain. The conditions associated with, or causal of, foot and ankle pain include inflammatory arthropathy, degenerative osteoarthropathy, posttraumatic arthrosis, entrapment neuropathy, tendinopathy, joint instability, soft-tissue pathology, and sequelae of congenital/developmental abnormalities. Less frequently, tumorous conditions, chronic infection, and vasculopathy produce symptoms in the foot and ankle.
The difficulty in locating the source of pain is often due to the compact nature of the foot anatomy: the close proximity of different spaces and structures, such as articulations and soft tissue insertions, challenge the clinician. Plain radiographs are poor indicators of the sources of foot pain1 and physical exam is of limited value in differentiating between two structures only millimeters apart. It is very important for the surgeon to locate the source of foot pain precisely in order to initiate treatment.2,3
The role of diagnostic imaging studies has a heightened impact on clinical practice when the source of foot pain is unknown or uncertain. The treating physician must know the diagnostic accuracy of imaging tests and recognize the efficacy of treatment based on that diagnostic accuracy. Arthrography and tenography of the foot and ankle have been applied routinely as diagnostic studies to determine anatomic abnormalities within joint or peritendinous space. Some authors have tried to predict disease activity and physical impairment based on arthrographic findings.4
Magnetic resonance imaging (MRI), computed tomography (CT), and ultrasound (US) have supplanted arthrography and tenography in rendering a visual diagnosis of anatomic abnormality. Therapeutic injection of joints and soft-tissue structures with local anesthetic and corticosteroids, performed by an orthopedist in an office, has important diagnostic significance.
The ability of local anesthetic to reduce pain is often a diagnostic procedure that locates the source of foot or ankle pain. One of the limited factors in the accuracy of such "blind" injections is the inability to recognize exactly where the medication was injected.3,5,6 Another source of diagnostic error is the possibility of a field block or regional nerve block by an un-guided injection, thereby masking the true site of pain origin.
Fluoroscopically guided injections using contrast material to confirm the position of the needle allows documentation of the exact site of injection, demonstrates communication between joints, or between tendons and joints, and outlines space-limiting lesions such as tendon sheath stenosis or limited joint volume.
Precise documentation of where the anesthetic is inserted is clinically very important, since any injection lacks specificity without knowledge of location. This has been well illustrated with injections in the peroneal tendon sheath and joints in the foot and ankle: anesthetic placed in the peroneal sheath may enter the ankle or subtalar joint thereby confusing the diagnosis.5
Diagnostic injections within joint spaces, surrounding tendons, and within bursae are useful localizers for planning surgical treatment. Several recent studies suggest that image-guided anesthetic injections increase the accuracy of diagnosis and have a positive influence on patient management, including decision-making by the clinician and the resulting patient outcomes.1,3,5,7 This paper describes short-term outcomes in three different foot conditions that have been studied with fluoroscopically guided injections–small joint arthritis, retrocalcaneal bursitis, and plantar fasciitis.
The purpose of this review is to establish awareness among radiologists and orthopedists that image-guided injection has several patient-care benefits, is a reliable diagnostic tool, and is an efficient use of imaging resources. In the outpatient clinic, there is an increasing role for the interventional musculoskeletal radiologist and modern imaging techniques.1,8,9
Materials and methods
Three groups of adult patients with foot pain were identified from the orthopedic foot clinic. All patients had foot and/or ankle pain and were evaluated by an orthopedist. The evaluation consisted of a problem-focused history, physical examination, weight-bearing foot radiographs, and follow-up examinations for a minimum of 3 months. All patients with Achilles tendon/bursitis symptoms had a magnetic resonance imaging (MRI) study. Three diagnostic groups were created: joint pain, plantar fascia pain, and Achilles tendon insertion pain.
Symptomatic and suspected painful small joints of the foot were further evaluated by arthrogram, including local anesthetic with contrast. Plantar fascia patients were evaluated by a perifascial injection, again, using fluoroscopic guidance and contrast solution in addition to the anesthetic. The Achilles tendon insertion group had fluoroscopic-guided injection of the retrocalcaneal bursa if the MRI showed signs of bursal inflammation.
Relief of pain was scored by the patient on a 0-to-10 visual analogue pain scale, with 0 indicating "no pain" and 10 "the worst pain imaginable." Clinical significance of the injection was determined by the immediate pain improvement >50% on the pain scale. Failure to improve or worsening of the pain was considered a negative result. Pain improvement between 0% and 50% was indeterminate, and for this study was not considered clinically significant in predicting surgical outcome. Statistical power and significance were not applicable to this first group of patients.
Results
In 96 patients evaluated for arthritis pain, 218 joints were injected (figure 1).
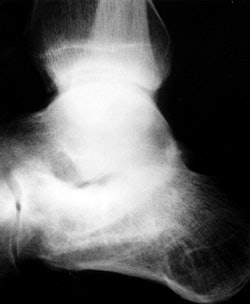
FIGURE 1. (A) Lateral radiograph of a patient with hindfoot pain and the suggestion of subtalar arthrosis.

(B) Sagittal fat-suppressed MR image showing posterior facet arthrosis of the subtalar joint and edema within the sinus tarsi.

(C) The patient undergoing a series of injections with contrast seen in the ankle and sinus tarsi. The ankle injection did not relieve symptoms, the sinus tarsi injection relieved 75% of pain.

(D) Lateral radiograph 10 months after talo-calcaneal fusion and excision of the sinus tarsi contents with a reported 80% reduction in pain.
All joints were injected successfully. Based upon the degree of pain relief from injection, 22 patients were offered surgical treatment and 18 people chose surgical treatment. There were 7 painful ankles and 11 painful feet in 18 patients that had surgical treatment. All of the painful small joints of the foot had arthrodesis, 3 of the painful ankles had arthrodesis, 2 ankles had synovectomy and 2 had replacement arthroplasty. Ten of 11 patients with foot arthrodesis had pain relief similar to that of the injection and 1 patient had approximately 50% pain relief.
The ability to limit the number of joints fused by assessing pain relief from a series of preoperative image-guided arthrograms was also important. All patients have a minimum of 9 months follow-up since surgery. Five of 7 ankle pain patients had relief similar to the injection; one ankle arthroplasty and one arthrodesis patient had 50% improvement, none were worse following surgery. All surgical pathology specimens from the arthrodesis sites demonstrated the pathologic tissue changes of chronic synovitis, degenerative joint disease (i.e., bone and cartilage degeneration), or both.
In 54 patients identified with pain at the origin of the plantar fascia, 47 had relief >50% of their pain by a single perifascial injection (figure 2).
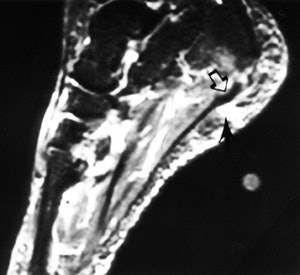
FIGURE 2. (A) This sagittal fat-suppressed MR image shows thickening of the plantar fascia origin (hollow arrow) and edema within the fat pad (black arrow), near a skin marker.
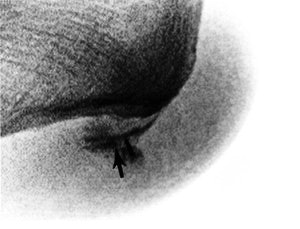
(B) The patient undergoing a fluoroscopy-guided injection with the contrast (black arrow) tracking along the fascia origin. The patient reported complete pain relief from the anesthetic.
There were no complications from injection, though three patients reported temporary worsening of the plantar heel pain. Surgery was recommended to eight patients with recurrent pain and successful pain relief from an injection. Five patients underwent excision of the origin of the plantar fascia and have been followed a minimum of 1 year. There were no complications from the surgery and all patients reported functional improvement, though none had pain relief equal to the maximum improvement from an injection. All five surgical pathology specimens demonstrated abnormality of the fascial tissue.
In 15 patients evaluated for Achilles tendon insertion pain, four patients had symptoms and findings of isolated retrocalcaneal bursitis with normal tendon. These four patients all had relief of symptoms following an injection to the retrocalcaneal bursa. Two patients had prolonged relief from the injection plus oral non-steroidal medication, two patients had recurrent symptoms and underwent surgery to excise the bursa and remove the underlying prominence of the calcaneus. Both operative patients reported improvement in pain and function at 9 months post-procedure that was very close to the level of comfort following injection. Review of the surgical pathology revealed acute and chronic inflammation of the bursa and no pathologic bone change in each case.
Discussion
Earlier published reports of image-guided small joint injection disclosed improvement in the surgeon’s confidence in the diagnosis, a positive effect on clinical decision making, and a beneficial effect on treatment outcome.3,5 The three diagnoses included in this manuscript suggest the efficacy of image-guided injection in the management of soft-tissue pain in the foot and joint pain in the foot or ankle. Other painful foot and ankle conditions are amenable to advanced imaging with MRI, CT, or ultrasound, followed by confirmatory injection.
Building on the improved accuracy of the clinical diagnosis of several different painful conditions, the surgeon may use the subjective improvement from an anesthetic injection to characterize the anticipated result from successful surgery. More study is certainly needed to determine the treatment efficacy of image-guided injections with corticosteroid or hya-luronic acid and to correlate patient outcome with pain relief from a guided injection.
Preliminary results suggest that the use of modern diagnostic imaging techniques have expanded from demonstrating a locatable abnormality to planning an interventional procedure that has treatment implications. Fluoroscopic-, US-, or CT-guided injection allows administration of an anesthetic as well as a therapeutic agent.8 If permanent pain relief is not achieved from image-guided injection of medication into a joint or bursa, the temporary pain relief caused by the anesthetic agent may be a prognostic indication of patient outcome with conventional orthopedic procedures.4,8,9
Since one source of uncertainty in failed surgery of the foot or ankle is the correctness of the diagnosis,7,8 image-guided injection should decrease the likelihood of poor surgical outcome due to inaccurate identification of the clinical source of preoperative pain.
With resources for health care and treatment innovation decreasing, orthopedic surgery for the management of painful foot conditions may provide significantly better outcomes with the inexpensive addition of image-guided injection. Future research into the efficacy of image-guided injections is needed to determine both the accuracy of diagnosis and the cost-effective prediction of surgical outcome. These prospective studies should investigate if fluoroscopy-guided or ultrasound-guided injections are more accurate, whether they are reasonable treatment modalities, and examine the relative cost of the two procedures.
There is now a growing body of evidence that the surgical care of painful foot and ankle conditions is yielding better patient outcomes due to better clinical information from advanced imaging techniques combined with the patient’s response to a guided injection of local anesthetic.
Dr. Hurwitz is an Associate Professor in the Department of Orthopedic Surgery, University of Virginia, Charlottesville, VA. Dr. Lucas is a Musculoskeletal Radiologist with Pittwater Radiology, Sydney, Australia.
References
1. Anzilotti K, Schweitzer ME, Hecht P, et al: The effect of foot and ankle MR imaging on clinical decision making. Radiology 201:515-517, 1996.
2. Grasel RP, Schweitzer ME, Kovalovich AM, et al: MR imaging of plantar fasciitis: Edema, tears, and occult marrow abnormalities correlated with outcome. AJR 173:699-701, 1999.
3. Lucas PE, Hurwitz SR, Kaplan PA, et al: Fluoroscopically guided injections into the foot and ankle: Localization of the sources of pain as a guide to treatment- prospective study. Radiology 204:411-415, 1997.
4. Kuper HH, van Leeuwen MA, van Riel PL, et al: Radiographic damage in large joints in early rheumatoid arthritis: Relationship with radiographic damage in hands and feet, disease activity, and physical disability. Brit J Rheumatol 36:855-861, 1997.
5. Khoury NJ, El-Khoury GY, Saltzman CL, Brandser EA: Intraarticular foot and ankle injections to identify source of pain before arthrodesis. AJR 167:669-673, 1996.
6. Mizel MS, Michelson JD, Newberg A: Peroneal tendon injection: Utility of concomitant injection of contrast material. Foot Ankle Int 17:566-568, 1996.
7. Fryback DG, Thombury JR: The efficacy of diagnostic imaging. Med Decis Making 11:88-94, 1991.
8. Mitchell MJ, Bielecki D, Bergman AG, et al: Localization of specific joints causing hindfoot pain: The value of injecting local anesthetic into individual joints during arthrography. AJR 164:1473-1476, 1995.
9. Steinbach LS: Painful syndromes around the foot and ankle: Magnetic resonance imaging evaluation. Topics Mag Res Imaging 9:311-326, 1998.
Let AuntMinnie.com know what you think about this story.

















