Using water as a conductor between a ring-shaped transducer and breast tissue, Michigan-based researchers are experimenting with ultrasound tomography for breast cancer screening. Benefits of this technique include the ability to scan dense breasts and a lack of radiation, according to the group.
"The water serves to couple the breast tissue and transducer, while allowing the breast to maintain a more natural shape without deformation or tissue displacement typically encountered in traditional mammographic or ultrasonic scanning," explained Carri Glide, Ph.D., a medical physicist with the Karmanos Cancer Institute in Detroit, who presented the results at the 2007 American Association of Physicists in Medicine (AAPM) meeting in Minneapolis. Study co-authors are also from Detroit-based Wayne State University.
With their method, the patient lies in a prone position, with a breast projecting down into a water bath. The device (called Computerized Ultrasound Risk Evaluation, or CURE) incorporates a transducer ring, with a diameter of 20 cm, which encircles the breast and translates downward, imaging from near the chest wall through the nipple region in intervals of 45-60 seconds.
The quality of an ultrasound exam is linked in large part to the skill of the operator. Glide told AuntMinnie.com that this technology does alleviate some of that operator dependence.
"Because our technique involves a ring transducer that translates independently, it is essentially an operator-independent imaging modality," she explained. "By contrast, conventional ultrasound relies upon the operator to direct the transducer wand toward the tissue in question."
 |
| The patient setup and clinical prototype of the Computerized Ultrasound Risk Evaluation (CURE) device. Above, prone patient positioning for the CURE scan. Below, close-up of the imaging tank showing the transducer ring affixed to a mechanical arm that steps the ring down while imaging the entire breast volume. |
 |
The ultrasound signal is sequentially transmitted by each element and subsequently received with all 256 elements situated around the ring. This sequence is then repeated for each transmitting element. Because of its circular transducer arrangement, the device captures most of the scattered, transmitted, and reflected field, which provides more information about the breast tissue compared to conventional ultrasound, which only detects a small fraction of the directly back-scattered field, Glide said. Using the transmitted ultrasound information, images are reconstructed for the entire breast volume.
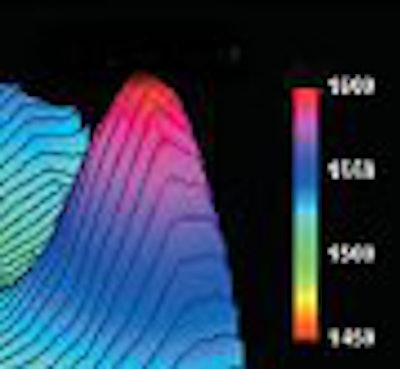
While testing their hypothesis that acoustical velocity could be used as a measure of breast tissue density, the researchers discovered a correlation between the speed of the sonographic wave transmitted and the density of that tissue. They found that the ultrasound tomography device could provide the definition needed to detect, characterize, and differentiate normal, benign, and malignant tissue through 3D visualization of submillimeter objects.
"The method is certainly safer because we use ultrasound, so there is no radiation risk associated with the scan," Glide said.
Another bonus is that breast tomography offers a more comfortable exam, according to Glide. "The technique is also painless because we do not use compression in our imaging. Instead, the breast is situated in the center of the transducer ring, and the ring does not typically even touch the patient, making it much more comfortable because patients do not undergo compression. Overall, the device has the potential to be more accurate, and that is what the clinical trials are designed to quantify," she said.
In a paper published earlier this year, Glide's group described the results of imaging 48 patients with an ultrasound tomography prototype. Each dataset was comprised of 45-75 tomograms ranging from near the chest wall through the nipple region. Whole-breast acoustic velocity was determined by creating image stacks and evaluating the sound speed frequency distribution.
The acoustic measures of breast density were evaluated by comparing qualitative and quantitative results to two mammographic density measures. The former involved a radiologist's visual assessment of each mammogram, while the latter required digitizing craniocaudal (CC) and mediolateral oblique (MLO) mammograms and implementing semiautomatic segmentation routines.
The researchers found an approximately 140 m/sec difference in acoustic velocity between the fatty and dense (BI-RADS) categories, with statistically significant differences in mean sound speed demonstrated between each category. In addition, an increased sound speed was exhibited with increased BI-RADS category. Moderately strong positive associations were demonstrated between mean acoustic velocity and quantitative measures of mammographic percent breast density for both MLO and CC views (r² = 0.65-0.76), respectively (Medical Physics, February 2007, Vol. 34:2, pp. 744-753).
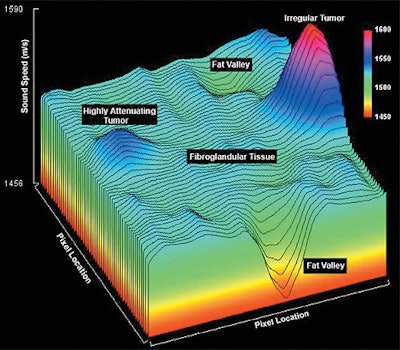 |
| The sound speed surface plot of a phantom image. The z axis is the sound speed in m/sec, and the x and y directions are the pixel locations. The increased sound speeds in the regions corresponding to the tumor-like regions and the fat valleys correlating with fat inclusions are also present. The legend in the top right-hand corner indicates the sound speed in m/sec. Glide C et al, "Novel approach to evaluating breast density utilizing ultrasound tomography," Medical Physics, 34 (2), 2007: 744. |
The researchers have since recruited additional patients for their clinical trial, and are halfway toward their recruitment goal of 300. Once they reach 300, they will do accuracy comparisons between their method and mammography, as well as standard ultrasound. Glide said that they hope to gain U.S. Food and Drug Administration (FDA) approval and introduce the device into general use.
"In terms of breast density, the current standard of care in breast density reporting involves a radiologist's subjective estimate based on a four-category scale," she added. "Clearly obtaining a quantitative number, as in volumetric breast sound speed, has the potential to be more accurate than a coarse and subjective scale. Also, the procedure is quick, taking less than a minute for the entire breast volume to be imaged."
In the e-mail interview with AuntMinnie.com, Glide clarified that the current clinical trials are evaluating the ultrasound tomography's role as an adjunct to mammography for all women of various breast densities. Multicenter trials will be required for FDA approval, she added.
Asked how ultrasound tomography differed from other investigative breast imaging techniques, such as breast tomosynthesis or elastography, Glide said that the ring transducer was the key.
"(The ring transducer) allows detection of directly reflected, scattered, and transmitted information. Because of this, our machine is multimodality, meaning that we can create two types of reflection images (with similar architecture to mammography) and use transmitted information to create both sound speed and attenuation images that represent changes in properties through the tissue," Glide stated. "Therefore, we get four types of images, all which can be used to give us information about the breast. We can also overlay the images with perfect registration -- a 'fusion' of our different image types. This is unique to our clinical prototype."
By Kathlyn Stone
AuntMinnie.com contributing writer
August 30, 2007
Related Reading
New techniques in breast ultrasound may find more cancers, March 1, 2007
Ultrasound continues to make inroads in breast imaging, February 6, 2007
Copyright © 2007 AuntMinnie.com