AuntMinnie.com presents the first in a series of columns on the practice of ultrasound from Dr. Jason Birnholz, an ultrasound veteran with more than 40 years of experience in this field.
Fellow UltraSounder,
Ultrasound exams are often requested for a specific clinical question and are limited to a particular organ or body part. However, medical conditions (including aging) have systemic consequences, and patients and their referring physicians may benefit greatly if flexibility is incorporated into exam protocols.
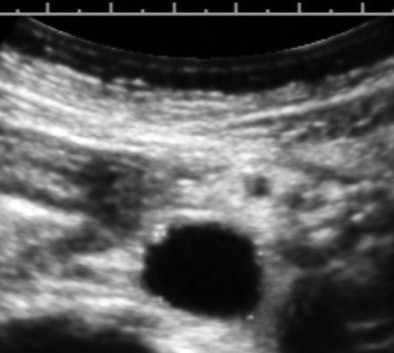
Here's a routine practice example that demonstrates the value of a medically centered exam technique. The image below is from the exam of an overtly healthy 47-year-old woman referred for heavy menstrual flow.
 All images courtesy of Dr. Jason Birnholz.
All images courtesy of Dr. Jason Birnholz.The image is a transverse cross-section of the distal abdominal aorta about 2 cm above the bifurcation. There are subintimal calcifications and a small plaque, which are distinctly pathologic, but now fairly common "incidental" findings at this woman's age.
Let's start with the way that we search for and perceive reflectivity, such as plaques or calcifications in the wall of a vessel. This is a contrast resolution task, which is identical to searching for a breast mass or looking for signs of placental senescence. Actually, contrast resolution search tasks are part of nearly all ultrasound exams.
Well-known technical factors affect image contrast, and we assume these are basic knowledge factors for ultrasound operators. These include center frequency, bandwidth, dynamic range, and display grayscale allocation settings. In addition, the eye has much better contrast distinction in color than in black and white. Many ultrasound machines have options for coloring images, which we will discuss in a later article since this is not a standardized practice.
For any instrument settings and inherent noise factors, contrast anomalies are best seen as cross-correlations between serial image planes (i.e., watching the screen while the probe is translated or scanned across the region of interest). This concept is really important, as it emphasizes that the exploratory ultrasound exam should be conducted as a live scanning survey. Once pathology is found, technical factors are optimized for the best possible still or representative image.
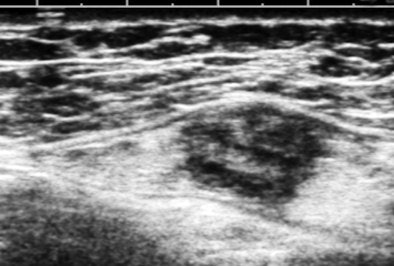
The image above is a breast cancer not suspected in screening mammography or physical exam in a woman referred for chest-wall pain (on the opposite side of the body). This lesion was found incidentally while scanning the upper outer quadrant of the left breast. The way we examine the breast is to think of the breast as a clock face with the nipple at the center, use a high-frequency array, orient the transducer perpendicular to a zone like a 2 o'clock radian, and slide the transducer from the nipple outward.
This suspicious nodule was immediately evident during continuous viewing. We decided to look at the breasts, because the patient had traveled some distance to get to us from a rural area with limited diagnostic resources and because she had expressed some anxiety about breast cancer.
Dynamic scanning
Being able to see the image in real-time is one of the most powerful aspects of ultrasound. It makes it easy to adjust the settings while you are looking at the image, and, of course, to optimize probe position. However, the fact that contrast sensitivity is so much better for moving pictures than for still ones is what really elevates ultrasound as a diagnostic imaging technique. In essence, dynamic viewing increases the signal-to-noise features for lesion detection; it's especially valuable when noise is high, such as when scanning through a lot of subcutaneous fat or with equipment that does not have speckle reduction.
In the early days of ultrasound, some facilities videotaped their exams with the thought that the interpreter could review the materials (at an increased real playback speed to save time) without being present during the exam itself. That never worked very well, and most radiologists during the videotape era realized that they needed to do some of the search part of each exam themselves.
A newer version of this notion is to do a digital save of a volume of interest with a 3D-enabled scanning unit. A remote interpreter can zip back and forth very quickly through a series of serial scan planes. However, the review may be limited to the single scan plane orientation. If the review is performed after the patient has left the facility and the opportunity to reconfirm a finding is lost, CT or MRI may be inappropriately utilized to resolve the interpreter's uncertainty.
This example also implies that in an exploratory exam, there is a necessary component of live viewing by an operator who has a technical knowledge base. The example was selected because a clinically important finding is well-removed from the pelvic viscera.
Scope
As I see it, the scope of the ultrasound exam is the most important issue facing ultrasound imagers today. Ultrasound education tends to focus on local signs of this or that form of pathology, and tends not to address the broader issues of what may be medically relevant to individual patients.
Why was the first patient referred for an exam? Excessive menstrual bleeding is a complaint. The patient's primary physician wants to know what the cause may be, but more exactly he or she needs to be certain, however unlikely it may be, that the patient does not have endometrial cancer.
Diagnosis is always prioritized by immediate danger and biological severity. We are all aware that metabolic syndrome has reached epidemic proportions, that clinical signs emerge 10 years or longer after the process has begun at a cellular level, and that women have been underserved with regard to preventive health measures for cardiovascular disease.
In this case, a small extension to the exam resulted in confirmation of an abnormal lipid profile and the initiation of aspirin and statins. By being informed of the finding, the patient has motivation for the behavioral changes that will presumably have a major impact on her life span. As for the bleeding, that was a simple polyp.
Logically, if an exam is done to exclude a major problem in one area, is it supportable that we not use the opportunity to evaluate problems that have high prevalence in the patient population, that are easily sought by ultrasound, and which have definite ultrasound findings? A very narrow clinical focus is a little like doing a chest x-ray and only looking at the right middle lobe of the lung and neglecting everything else. Scanning through the distal aorta probably adds 30 seconds to a pelvic ultrasound exam, hardly any time at all.
It's up to every facility to set a protocol for what an exam should include, hopefully with flexibility to account for specific patient needs as they become known during the study. Because of the nature of the ultrasound imaging process, every study needs to be thought of as a medical exam, and we always need to remind ourselves why the exam is being done: It is always for the greater benefit of the patient.
At times, ultrasound exams are requested by physicians who may not understand our diagnostic capabilities. The request may be addressed by a sonographer, who fulfills it as well as he or she is able but without the medical guidance from within the ultrasound facility to decide what is in the patient's best interest. These referral and exam scope issues are all too common in busy facilities that are understaffed and underreimbursed. I do believe that injecting clinical flexibility and thinking about why we do every exam can only serve to increase our usefulness and performance for whatever clinical application of ultrasound we may pursue.
Dr. Jason Birnholz is a graduate of the Johns Hopkins University School of Medicine and performed his first scans in 1968 while serving as a fellow at the National Institutes of Health. He started the ultrasound service at Massachusetts General Hospital in 1971, and he tested and introduced phased-array ultrasound imaging at Stanford University Medical Center in 1975 and computed sonography at Rush Medical College in 1983. He has been radiologist-in-chief at the Boston Hospital for Women, chief of the ultrasound section at Brigham and Women's Hospital, and professor of radiology at Harvard Medical School. He is also the founder and chief of Diagnostic Ultrasound Consultants in Oak Brook, IL.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.