It is generally radiology that sets the precedent as to when and where a particular modality is used, and other specialists follow suit. But in the case of ocular imaging, radiologists might consider taking a glance at what ophthalmologists are doing, according to a group from the University of Texas M.D. Anderson Cancer Center in Houston.
"Although MRI of the eye is favored by radiology, sonography of the eye is used by ophthalmology subspecialists to evaluate the posterior eye," wrote Dr. Deepak Bedi in a poster presentation at the 2004 American Roentgen Ray Society (ARRS) in Miami Beach, FL. Bedi, as well as co-investigators Drs. Chaan Ng and Sanjay Singh, are radiologists; Dr. Dan Gombos is an ophthalmologist.
That's because ultrasound actually offers better cross-sectional anatomy of the entire ocular globe, the group explained. In an interview with AuntMinnie.com, Bedi added: "We made it a point in the poster not to compare MRI and ultrasound. But the actual resolution on ultrasound is better than it is on MRI, which is generally considered the best investigation that you can do," he said. "If you look at the physics of ultrasound, and the way the image is formed, it gives you more detail on a much larger scale."
Based on recent ocular health predictions in a graying U.S. population, neither radiologists nor ophthalmologists can afford to be short-sighted in their approaches to eye imaging. According to the Eye Diseases Prevalence Research Group (an initiative of the National Eye Institute, National Institutes of Health), the incidence of cataracts and age-related macular degeneration (AMD) is expected to increase dramatically in the next 20 years (Archives of Ophthalmology, April 2004, Vol. 122:4, pp. 451-452).
Currently, AMD is the most common cause of blindness in Caucasian adults, while glaucoma and cataracts are more likely to cause sight loss among African-Americans (Archives of Ophthalmology, April 2004, Vol. 122:4, pp. 564-572).
AMD and cataracts have also been linked to an increased risk of death, based on the NIH's Age-Related Eye Disease Study (AREDS). The hypothesis is that eye disorders reflect other systemic, as well as local, disease processes (Archives of Ophthalmology, April 2004, Vol. 122:4, pp. 716-726).
Eye conditions have also been tied to heart attack patients who are treated with balloon catheters and stents (British Journal of Ophthalmology, April 2004, Vol. 88:4, pp. 494-496).
For their ARRS exhibit, the group offered a broad overview on the application of eye ultrasound to recognize normal structures as well as abnormalities, particularly tumors.
Technique
The radiologists used conventional grayscale ultrasound with 7.5-15-MHz transducers (Siemens Medical Solutions, Malvern, PA), supplemented with color Doppler. The patient was supine with the eyelid closed. A small amount of gel was used to evaluate the posterior eye. For looking at the anatomy of the anterior chamber, they recommended more gel or a standoff pad. A B-mode probe was used for open-eye imaging.
Because a linear transducer was used, the images were in the traditional anterior-to-posterior orientation.
In comparison, the ophthalmologist used a 10-MHz transducer (Innovative Imaging, Sacramento, CA) specialized for eye imaging with an A-mode probe. Because this is a sector transducer, the images were rotated to a left-to-right orientation. The difference is purely technical, Bedi explained, because opthalmologists work with A-mode probes, which generate images on the monitor that are better read left-to-right.
Either way, the blink reflex was paralyzed and there were no complaints from the subjects, the group stated.
Best on US
The areas of the eye that can be visualized with ultrasound are the sclera, the posterior ciliary arteries, and the lens, although the latter can be inspected directly without imaging. However, the presence of a mature cataract of the lens may not allow inspection of the retina or optic disc, which could necessitate ultrasound.
Other eye regions that can be seen are the vitreous body (anechoic appearance), the choroids point of the uveal tract, the ciliary body, and the iris. Ultrasound is useful for diagnosing choroidal melanoma and metastatic tumor. The optic nerve, the central retinal vessels, and other retinchoroid vessels were recognizable.
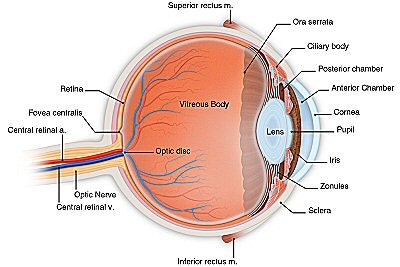 |
| Anatomy of the normal eye. Illustration courtesy of the American Academy of Ophthalmology. |
The group cautioned that there are ocular regions where ultrasound's performance is lackluster, including the cornea, conjunctivae, and the posterior chamber. Also the retina, choroid, and sclera will be perceived as one layer on ultrasound, rather than distinct areas.
Disease processes
Ultrasound is especially useful in a pediatric population because it does not require sedation, Bedi and colleagues noted. They cited a case of rhadbdomyosarcoma, a malignancy of the orbital cavity that can be treated with radiation and chemotherapy. In addition to relying on ultrasound for the initial diagnosis, the group reported that using sonography for follow-up meant that "sedation for repeated CT/MRI...was avoided in this child."
 |
| A cone-shaped rhabdomyosarcoma (arrowheads) is seen in the orbit behind the eyeball. The optic nerve (black arrow) is partially encased by the tumor. Note the retinal detachment (white arrow) in the eye. The patient was a five-year-old child. Ultrasound imaging made it unnecessary to perform MRI, which would have required sedation. |
Other diseases that were readily differentiated in ultrasound were malignant melanoma and its changing appearance after treatment; metastases from breast and lung cancer; retinoblastoma, and lymphoma. Sonography depicted the latter as flat echogenic masses.
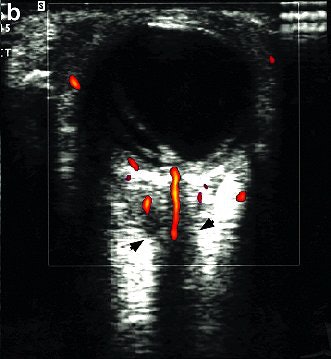 |
| Color Doppler ultrasound shows that despite encasement of the optic nerve by tumor, the blood flow is intact to the posterior eyeball through branches of the short posterior ciliary arteries and the central retinal artery. Images courtesy of Dr. Deepak Bedi. |
"Color Doppler and A-mode ultrasound are invaluable for characterizing masses," they pointed out. "The ultrasound exam is rapid, cost-effective, has no contraindications, such as pacemakers in MRI. It avoids the irradiation associated with CT and the need for sedation in children."
An eye for an eye
Ultrasound of the eye has never been the rope in the tug-of-war between radiologists and ophthalmologists. Historically, eye experts have kept to more "low-tech" ultrasound techniques, while imaging specialists have gravitated toward more sophisticated modalities.
"I think it's a question of familiarity," Bedi said. "MRI is universally available in this country. There is no shortage of MRI and no shortage of money spent on it.
For ophthalmologists, (eye ultrasound) is a natural extension of their physical exam so it's never really come to be a turf issue. Radiologists are still not interested in doing ultrasound. They've just got too many other things going on."
Which is unfortunate, as radiology departments have the more advanced machines for eye imaging, including high-resolution capability and color Doppler -- equipment that most ophthalmologists are not working with yet, Bedi said.
Because radiology has the technology, and ophthalmology has the know-how, the current situation is a prime opportunity for collaboration. At M.D. Anderson, ultrasound is used routinely by both groups with great success, Bedi said. Future shifts in eye health trends, such as the growing incidence of AMD cases, could also call for more inter-specialty imaging.
"Presumably, in AMD, blood flow to the retina plays a role, and we can use Doppler to look at the blood flow and the retina at the back of the eye," Bedi speculated. "The role that I see for ultrasound involves contrast media and then looking at the eye, and the blood flow in the retina, to see if there are differences that you can pick up in perfusion. Maybe you can quantitatively assess normal flow versus abnormal flow."
However, performing ocular sonography will require some adaptation on the part of radiologists, Bedi noted.
"When ultrasound is done, in 80%-90% of the clinical situations, the technologists do the exam," he said. "(Eye ultrasound) really does require the physician to actually go and do the scan."
By Shalmali PalAuntMinnie.com staff writer
May 25, 2004
Related Reading
Interventional radiologists may be at risk for posterior subcapsular cataracts, March 30, 2004
Radiotherapy plus thermotherapy provides good local control of uveal melanoma, July 26, 2002
MRI trains an eye on orbital Lyme disease, June 10, 2002
Copyright © 2004 AuntMinnie.com