A software tool can swiftly and accurately perform semiautomated volumetric quantification of pleural effusions on MDCT studies, yielding significant time savings over manual quantification methods, according to researchers from Northwestern University.
In a study of 29 pleural effusions, a team led by clinical research associate Dr. Marcos Botelho found that semiautomated volumes were statistically similar to those generated manually and had high interrater agreement. Average user time was also nearly four minutes faster using the semiautomated volumetry software.
"Semiautomated segmentation of pleural effusions is feasible and reproducible, and can be considered fast and precise when compared to the gold standard, which is manual segmentation," Botelho told AuntMinnie.com.
He presented the team's research during a scientific session at the European Congress of Radiology (ECR) earlier this month in Vienna.
Pleural effusions are among the most frequent findings in clinical practice. They are initially evaluated mostly based on radiography or ultrasound. CT may be regarded as beneficial, though, when effusion size will affect the decision to perform thoracocentesis, Botelho said.
"However, tomographic evaluation of effusion size is mainly subjective, often described as small, moderate, or large," he said.
Because the Northwestern group has significant experience in volumetric evaluation of body lesions, they thought it would be interesting to utilize a semiautomated tool to provide clinicians with volume data on pleural effusions in an objective and fast manner, which could be helpful in patient management, Botelho said.
To test this approach, the team studied 29 consecutive pleural effusions in 20 adult patients receiving contrast-enhanced chest MDCT. Two independent and blinded readers then employed semiautomated segmentation software (Vitrea, Vital) to estimate pleural effusion volume. The researchers also obtained manual volumetry to serve as the gold standard for the purposes of the study.
Botelho and colleagues then evaluated the volumetry results for precision, assessment time, interrater agreement, and percentage of over- and undersegmentation. The two radiologists obtained very similar volume measurements for effusions; Bland-Altman precision of 8.2% shows high reproducibility for the software, he said.
| Manual vs. semiautomated segmentation | |||||
| Manual segmentation | Semiautomated segmentation | p-value | |||
| Mean effusion volumes | 1033.1 mL | 1040.3 mL | p = 0.379 | ||
| Mean user segmentation time | 336 sec | 105.3 sec | p < 0.001 | ||
The mean volumes obtained with most methods were statistically similar, showing Bland-Altman precision of 5% and a Lin's concordance correlation coefficient of 0.998. The semiautomated software did have a mean of 2.3% oversegmentation.
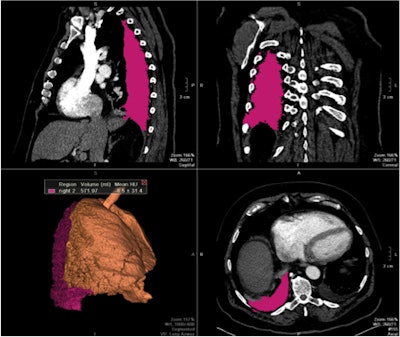 |
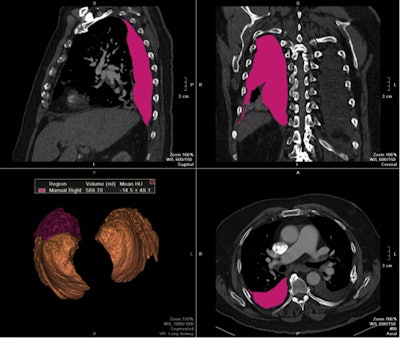
| Images show three traditional multiplanar reformatted reconstructions (MPRs) and one 3D reconstruction of final segmented pleural effusion volumes using a semiautomated quantification method (above) and manual method (below) on the same patient. The semiautomated segmentation method calculated a pleural effusion volume of 571.97 mL, a difference of less than 3% compared with 589.79 mL on manual segmentation. All images courtesy of Dr. Marcos Botelho. |
 |
In the next phase of the work, Botelho and colleagues would like to test the method in a larger patient cohort, as well as correlate the results with findings of other software tools. The researchers believe their results will be reproducible with other software packages, he noted.
"Also, it would be interesting to test the precision and reproducibility of semiautomated segmentation software to evaluate volume in specific clinical situations, such as in patients with hemothorax and empyema," Botelho said. "One other idea is to try and implement the estimated volume in the chest reports and, in the future, correlate if the information impacted the decision of performing the thoracocentesis or not."