While much of the recent concern over medical radiation dose has focused on CT, fluoroscopy is another imaging modality that can pack a radiation wallop. In some cases, patients are leaving the fluoroscopy table unaware that they've received enough radiation to cause skin injury.
The problem is compounded by the fact that current guidelines on fluoroscopy-induced skin injury are 16 years old and have been in need of updating, according to Stephen Balter, Ph.D., of Columbia University Medical Center in New York City. Balter led a multicenter team commissioned by the National Council on Radiation Protection and Measurements (NCRP) that has published a new study updating the current state of clinical understanding of fluoroscopy-induced skin injury. The study was published in the February 2010 edition of Radiology (Vol. 254:2, pp. 326-341).
Balter and colleagues hope the new paper will help radiologists avoid cases of radiation-induced skin injury, and, when injuries do occur, recognize them more quickly so patients can receive treatment.
Rising incidence
The rapid growth of interventional radiology starting in the early 1990s has led to a concomitant increase in fluoroscopy-induced skin injury as patients are being left under the x-ray beam for longer periods of time. Fluoroscopy-guided interventions in most cases result in lower patient morbidity and faster recovery than open surgical procedures, but they have the potential to cause major skin injury, according to Balter.
"We think that as interventional radiology grows and displaces more major surgical procedures, there is a strong potential for increased injuries," he said in an interview with AuntMinnie.com. "The physician's ability to do more complex procedures is advancing faster than industry's ability to reduce the dose rate."
In many cases, neither patients nor clinicians are aware that a skin injury has occurred until days or even weeks after the interventional procedure, when telltale skin damage becomes visible. Some patients are baffled by the injuries, as they either weren't told or had forgotten that their fluoroscopy-guided study involved the use of radiation. In some cases, skin reactions have been attributed to defibrillator pads or grounding electrodes used for electrocautery.
"Some patients have no idea that their injuries were caused by radiation, so they get mistreated for more than a year," Balter said. "The referring physician has no idea, the patient has no idea. A month later they have something on their back and it's a puzzle to both of them, and off they go to a biopsy. And if it's major class 4 skin injury it's the worst thing you can do. You've biopsied damaged tissue that never heals."
 |
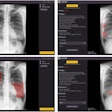
| Sequence of images shows progression of radiation injury in 40-year-old man who underwent multiple coronary angiography and angioplasty procedures. Image at left is six to eight weeks after exposure and shows prolonged erythema with mauve central area, suggestive of ischemia. Image at center is 16 to 21 weeks following exposure; depigmented skin with central area of necrosis is seen. At right, image at 18 to 21 months shows deep necrosis with atrophic borders. This sequence is available on the U.S. Food and Drug Administration (FDA) Web site and is in the public domain. |
Updating guidelines
In recognition of the problem, the NCRP in the fall of 2007 held a meeting at its headquarters in Bethesda, MD, with the goal of investigating radiation safety in fluoroscopically guided interventions. Balter and his group was tasked with reviewing and updating the last set of fluoroscopy radiation guidelines, issued in 1994 in a paper by Louis Wagner, Ph.D., from the University of Texas in Houston and published in the Journal of Vascular and Interventional Radiology.
Balter and the other committee members -- including Wagner -- found that the 1994 guidelines no longer accurately reflect what's known about the mechanisms of radiation-induced skin injury. For example, they rely heavily on exposure time as an indicator of radiation overexposure. While this seems logical, it can overlook the healing properties of the skin, which means that radiation delivered in one session can be worse than the same radiation dose delivered over multiple sessions.
Also, the reliance on fluoroscopy time ignores the fact that other imaging techniques, such as digital subtraction angiography (DSA) and cine mode, are often used during interventional procedures and deliver much different dose levels than conventional fluoroscopy over the same time period.
The older guidelines also don't take into account the differences in radiation dose required to penetrate thin versus heavy patients, with heavier patients requiring more dose. Finally, the 1994 guidelines included a table that gave the impression that 2 Gray (Gy) was the threshold of radiation at which skin damage would begin to appear. Balter and colleagues feel that this threshold overstates the effects of radiation for most patients, and that 3-5 Gy is probably more accurate. The group doesn't believe that effects below 5 Gy are of any long-term clinical significance.
To replace the 1994 guidelines, Balter's group has proposed a new table to govern radiation exposure, based on "bands" of skin exposure. Essentially, each band advises clinicians on the type of skin damage they'll see for that level of radiation dose, and how the injuries will evolve over time.
The current paper also details the types of skin reactions that can occur and when to look for them, and it includes a number of case studies of patients who received skin injuries from interventional radiology procedures.
Preventing radiation injuries
Because Balter's paper was designed to focus on the biology and signs of radiation overdose, it doesn't deal with methods for reducing radiation injury -- much of that guidance can be found in a paper by Stecker and colleagues in the July 2009 edition of the Journal of Vascular and Interventional Radiology. Stecker's paper advises interventional radiologists to tell patients before they leave the facility whenever a substantial amount of radiation is used. Balter's committee is working on a follow-up paper to be published in Radiology that will also include additional guidance on operational issues.
Balter's department has a nurse follow up by telephone if they don't hear back from patients. He also advises making sure that all physicians performing interventional procedures at a hospital be appropriately trained in fluoroscopy. Balter believes that the hospital privileging process can be one of the most effective tools for encouraging physicians to have the proper level of training.
Making progress
Balter cites some positive developments in reducing radiation dose. Vendors have made great progress in reducing the rate of radiation dose their machines deliver, thanks to technologies such as beam filtering, more intelligent programming, better beam management, and the conversion to flat-panel digital detectors. Balter estimates that new fluoroscopy systems deliver a dose rate that's 50% lower for the same-sized patient compared to older models.
Also, for the past several years, the U.S. Food and Drug Administration (FDA) has required every new fluoroscopy unit being sold in the U.S. to have dose monitoring tools. In addition, Balter's upcoming paper will have additional guidelines that update existing International Electrotechnical Commission (IAC) standards, such as requiring dose numbers to be visible on the machine during procedures.
Finally, a new DICOM object -- Radiation Dose Structured Report (RDSR) -- is being developed to provide automated dose reporting, making it easier to determine how much dose a patient received. Interventional radiology will be the first covered, with CT close behind, Balter said.
Despite rising concerns about dose, Balter points out that many of the patients being treated with interventional radiology are already sick, and many are older -- and older patients have one-third the risk of developing a radiation-induced cancer than children and young adults.
Radiation should be just one factor that physicians consider when deciding whether to use an interventional radiology procedure or conventional open surgery.
"Physicians should consider the short- and long-term outcomes, including the use of radiation, when deciding what kind of procedure to recommend to their patients," Balter said.
By Brian Casey
AuntMinnie.com staff writer
February 18, 2010
Related Reading
FDA launches initiative to rein in medical radiation, February 9, 2010
Congress sets hearing to review medical radiation, February 8, 2010
NIH tells scanner suppliers to include radiation monitoring, February 1, 2010
FDA finds new cases of radiation overexposure, December 7, 2009
NEJM study: Imaging procedures, radiation growing, August 26, 2009
Copyright © 2010 AuntMinnie.com